Review Article - Modern Phytomorphology ( 2025) Volume 19, Issue 5
The role of pharmacy in integrating herbal medicine: From patient counseling to quality control of natural products
Khalid Mohammed Refi1*, Khaled Farhan Albusaysi2, Turki Muteb Alharbi1, Nader Farhan Albesisi3, Rasha Mohammed Alghamdi3, Munifah Homud Alharbi3 and Ayidh Saad Alharthi12Prince Mohammed bin Abdulaziz Hospital, Ministry of National Guard, Saudi Arabia
3King Saud University Medical City, Saudi Arabia
Khalid Mohammed Refi, National Guard Health Affairs, Madina, Saudi Arabia, Email: refikh@mngha.med.sa
Received: 24-Aug-2025, Manuscript No. mp-25-171490; , Pre QC No. mp-25-171490 (PQ); Editor assigned: 28-Aug-2025, Pre QC No. mp-25-171490 (PQ); Reviewed: 02-Sep-2025, QC No. mp-25-171490; Revised: 05-Oct-2025, Manuscript No. mp-25-171490 (R); Published: 10-Oct-2025, DOI: 10.5281/zenodo.17774884
Abstract
The adoption of herbal medicine into the mainstream pharmacy practice is an increasing need, considering the fact that the use of natural products by patients has escalated alongside the use of conventional drugs. Pharmacists are crucial to the safe use of the products, evidence-based counseling, and quality control of herbal products. Nonetheless, a lack of knowledge, differences in the product quality, and inconsistencies in the regulations provide challenges to this integration. This paper discusses the knowledge, perceptions, and practices of the pharmacists in relation to herbal medicine and analyzes some of the current strategies of quality control. It is a synthesis of the evidence of surveys, systematic reviews, and laboratory studies done. Findings indicate that pharmacists are not very confident in herbal counseling, not well trained, and more often than not patients fail to inform pharmacists on their use of herbs. The quality assessment research indicates that herbal products sold in the market include adulteration, contamination, and low consistency in their potency. At the end of the paper, it is suggested to implement larger pharmacy curricula on natural products, the implementation of sophisticated methods of quality control, and the political regulations requiring standardized testing.
Keywords
Herbal medicine, Pharmacists, Patient counseling, Quality control, Herb–Drug interactions, Natural products, Pharmacovigilance
Introduction
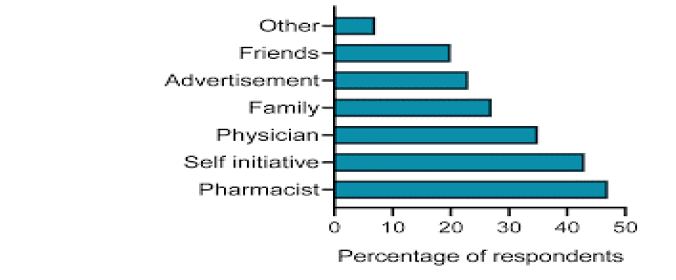
Herbal medicine is one of the most ancient types of therapy, but nowadays its application has become more active. In the United States, over 35 percent of adults are reported to use at least one herbal product and in some areas of Africa and Asia, medicine plants are used by nearly 80 percent of the population (Souza-Peres, et al. 2023). This is a trend that is used as a universal view of herbal remedies being more natural and thus safer. Nonetheless, this assumption has been over and over again refuted by reported Herb Drug Interactions (HDIs), and adulterated formulations (Stayduhar, et al. 2023).
Pharmacists are well placed to join the gap between the traditional and modern medicine. Being the most approachable healthcare providers, they communicate with patients almost every day and most of them do not mention the herbal use of products (Almeida, et al. 2025). This poses a safety risk, especially when the use of the herbal medicines has a potentiation effect with the traditional treatments as was the case with St. Johns wort and oral contraceptives and immunosuppressants (Souza-Peres, et al. 2023). In addition to counseling, pharmacists can aid in the quality management of Interviews revealed lack of structured s by means of pharmacovigilance and the identification of poor-quality products, as well as, promotion of more stringent regulations (Devi, 2025).
This paper examines how pharmacy can be used in the integration of herbal medicine and it is based on two major aspects, patient counseling and quality control of natural products. It focuses on the evidence collected since 2021, pointing out to both opportunities and challenges.
Scope of the study
This paper explores:
• Pharmacists’ roles in patient counseling: Their knowledge, perceptions, and communication practices regarding herbal products.
• Quality control mechanisms: Current analytical methods, regulatory frameworks, and pharmacy’s contribution to detecting adulterated or mislabeled herbal drugs.
• Global comparisons: Case studies from regions where herbal medicine is prominent (e.g., Nigeria, Latvia, Canada).
• Gaps in knowledge and practice: Lack of formal training in pharmacy curricula, insufficient pharmacovigilance systems, and variability in quality standards.
Justification
Although there is an increasing trend in the consumption of herbal medicines, pharmacists are not ready to handle their incorporation in the management of patients. According to the surveys, only 1/3 of community pharmacists are confident about herbal medicine counseling (Carr, et al. 2022). Additionally, the quality assessment research indicates that almost 40 percent of the samples of commercial herbal products do not contain the mentioned active ingredients or have adulterants (Quality Evaluation Study, 2022). Patients risk adverse reactions and therapeutic failure when not involved in counseling and product evaluation by pharmacists.
Based on these facts, this study is timely and needed. It places pharmacists not as dispensers of traditional medicines only but as arbiters of criticality with regard to patients, herbal systems of medicine and regulating bodies.
Literature Review
Pharmacists’ knowledge and perceptions
Stayduhar, et al. 2023 used a thorough evaluation of knowledge and perceptions held by U.S. pharmacists as well as pharmacy students based on herbal supplements. The research found out that the median quiz score of the licensed pharmacists and the students was 50 and 45 respectively which showed a big difference in objective knowledge on herbal medicine. Although the use and dispensing of herbal products are very common among patients, most pharmacists had a weak grasp of their pharmacological effects, therapeutic use, and adverse effects. Participants who had undergone some previous training or had undertaken some continuing education on herbal medicine had significantly increased confidence in counseling. Nevertheless, the researchers noted that the majority of the pharmacy curricula lacks compulsory courses on herbal products, which creates the endemic gap between the knowledge acquired in theory and its application in practice. This is a worrying aspect considering the fact that pharmacists usually deal with patients first before they seek advice on over-the-counter herbal remedies. Lack of knowledge can result in pharmacists giving incomplete and/or incorrect information unintentionally, which can lead to a greater possibility of herb-drug activity or poor therapeutic effect. It was also noted in the study that confidence is not conflicted with competence since some of the pharmacists who reported feeling confident failed to answer questions about certain interactions or dosage correctly, which underscores why more structured education and evidence-based sources are absolutely vital.
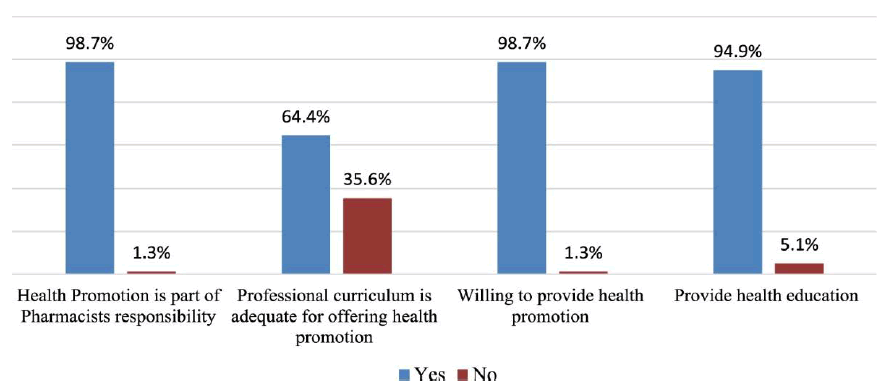
This has also been observed in Nigeria where a study by Almeida, et al. 2025 was done to evaluate the practices of community pharmacists as regards herbal medicines. The results showed that more than three out of four pharmacists regularly dispensed herbal products but less than half of them could easily describe the correct dosages or find possible interactions with conventional drugs. Personal experience or anecdotal knowledge was left to most pharmacists without trying to check its validity which posed a great threat to patient safety. This gap is further complicated by the fact that there is a scarcity of standardized guidelines or decision support tools at the community pharmacies. The two studies emphasize the importance of the necessity of the ongoing professional development and the curricular revision in order to impart pharmacists with the skills required to ensure safe and evidence-based counseling. Specific training initiatives and incorporation of training in pharmacy education on herbal medicine would help eliminate these knowledge gaps and provide pharmacists with the necessary skills to effectively engage with patients undergoing herbal treatment (Tab. 1).
| Study and Country | % Confident in counseling | % Routinely asking about herbal use | Median knowledge score |
| Stayduhar et al. (2023), USA | 38% | 22% | 50% |
| Carr et al. (2022), Global | 34% | 28% | N/A |
| Almeida et al. (2025), Nigeria | 42% | 31% | N/A |
Table 1. Pharmacists’ knowledge and confidence in herbal counseling (Selected studies 2021–2025).
Barriers to counseling
Bakhit, et al. 2021 have performed a systematic review to identify the challenges encountered by pharmacists when offering herbal medicine counseling. This review revealed three significant barriers, which always restricted the effective pharmacist engagement: The absence of formal training, the lack of evidence-based resources, and time constraints in the high-demand pharmacy environment. Most pharmacists indicated that they were not ready to respond to questions posed by patients correctly and offer consultations about possible herb-drug interactions. Poorly organized education at the pharmacy school and the little in terms of continuing professional development were pointed out as the key factors that enhanced this knowledge gap. The pharmacists in most cases are left to use personal experience, anecdotal reports or information provided commercially and this might not be scientifically proved. Not only does this condition influence the quality of the counseling, but it can as well influence patient safety, incomplete or incorrect counseling can have negative consequences, decrease therapeutic effectiveness, or pose a threat to prescription drugs. Bakhit, et al. 2021 also noted that such barriers should be overcome through a complex strategy that involves curriculum changes, professional development courses, and implementation of reliable and evidence-based instruments in pharmacy care.
Souza-Peres, et al. 2023 also presented the notion of herbal counseling experiences of Canadian pharmacists and serve to illustrate the challenges outlined in the systematic review. The reason as to why most participants were not ready to counsel patients on herbal products was the unavailability of authoritative and centralized databases on herbal products. Pharmacists were also concerned that in the absence of confirmed and updated information, they could end up unknowingly jeopardizing the safety of patients. Time was also a very critical factor; busy community pharmacies usually restrict the time one can consult on the use of herbs in a proper manner. Practically, it implies that the pharmacists can give short and generalized advice, or evade the subject matter even though the patients already take herbal supplements in addition to conventional drugs. This evidence supports the necessity of broad interventions that provide pharmacists with knowledge and practical tools that they could use to safely incorporate herbal medicine counseling in their daily activities. These barriers can be minimized through access to evidence-based resources, specific consultation time, and organized training sessions that would ultimately increase pharmacist confidence and efficiency in patient-centered care (Fig. 1).
Figure 1. Reported barriers to herbal counseling among pharmacists. Note: Bar graph with three main categories: Lack of training (65%), Lack of evidence resources (52%), Time constraints (43%)
Patient safety and herb–drug interactions
Herb-Drug Interactions (HDIs) remain a major issue of patient safety since it may modify the pharmacokinetics of traditional medication and cause treatment failure or side effects. A good-known example, which is well documented, is the use of St. John wort as an antidepressant, which is a herbal preparation, which increases Cytochrome P450 (CYP) enzymes, most notably, CYP3A4. This induction increases the metabolism of various prescription drugs, such as immunosuppressants, such as cyclosporine, oral contraceptives, and some anticoagulants (Souza-Peres, et al. 2023). The clinical implications are severe: When the levels of immunosuppressants in the plasma are lower, the chance of organ transplant rejection consequently grows, whereas the diminished power of oral contraceptives may lead to unintended pregnancies. Likewise, grapefruit juice, which is typically taken as a component of a healthy diet, is an inhibitor of CYP3A4 enzymes, resulting in higher blood concentrations of drugs like statins, which predisposes to myopathy and liver toxicity. Such cases indicate that pharmacists should know about common and less frequently mentioned HDIs because not all patients will regard herbal products or food as drugs that should be disclosed.
Interaction of herbal and conventional medicine is also a factor that affects patient safety, in terms of what the general population thinks about the two. In 2022, a survey of Latvian citizens showed that the majority of the population was worried about the combination of herbal products with prescription drugs, especially in the case of patients with cardiovascular diseases (Karklina, et al. 2022). However, in spite of such knowledge, most patients still take herbal treatments in conjunction with prescribed treatments without consulting a medical practitioner. To narrow this gap in knowledge, pharmacists can have a key role to play by participating actively by inquiring about herbal consumption, offering evidence-based advice and checking on possible interactions. Communication is crucial since even natural substances that are widely used such as ginkgo biloba, garlic, or valerian may have an interaction with anticoagulants, antihypertensives, or even sedatives. These results underscore the fact that HDIs are not purely theoretical threats they are real challenges that may be overcome only through the active participation of pharmacists who have to guarantee patient safety, as well as therapeutic effectiveness (Fig. 2).
Figure 2. Common herb–drug interactions relevant to pharmacy practice.
Quality control challenges
The examination of commercially available herbal products is always chaos with numerous chemical cases indicating the presence of a high number of quality problems, which pose a health, performance, and consumer confidence concern. To provide an example, Nandre, et al. 2022 checked ginseng supplements sold in the United States and found out that 36 percent of the assessed products had a concentration of ginsenoside, the main bioactive constituent of the herb, lower than half of the stated one. This underdose may make the products inefficient especially to patients who use ginseng to treat conditions like fatigue, diabetes or memory lapses. Another issue that was revealed by the study was the variability among batches of the same brand implying that there was no consistency in the manufacturing process and lack of quality control mechanisms. These results indicate that even well-known and controlled herbal products can be affected by inconsistencies that may undermine patient results. Pharmacists should, therefore, be careful in recommending or dispensing herb products and they should be ready to advise the patient about the inconsistency of the products in terms of potency and to advise the patient on the need to use herbs produced by a well-known manufacturer.
Similarly, a European quality assessment study indicated the use of synthetic sildenafil in various commercialized natural sexual enhancement items (Quality Evaluation Study, 2022). The process of herbal products and pharmaceutical agents is also quite worrisome as the end consumer is exposed to potentially hazardous chemicals without necessarily being aware of it and such chemicals may interact with other medications or aggravate existing health disorders, including hypertension and cardiovascular disease. Other studies have also recorded cases of heavy metal contamination, pesticides or even unlabeled pharmaceuticals, which illustrates the problem at large of product safety in the herbal supplement market. These observations underscore the importance of pharmacists in counseling and monitoring of patients. Learning about typical adulteration and encouraging strict testing measures, pharmacists can contribute to the reduction of risks and provision of safe, effective, and genuine herbal products to patients. In addition, further innovations, like incorporating the use of analytical procedures like High-Performance Liquid Chromatography (HPLC), DNA barcoding, and metabolomic profiling into the regulatory systems, maalso help to improve the quality of the products and increase the level of trust in herbal medicine among the populace (Tab. 2).
|
Product |
Country |
Quality Issue |
Source |
|
Ginseng capsules |
USA |
Sub-therapeutic active ingredient |
Nandre et al. (2022) |
|
Sexual enhancers |
EU |
Adulterated with sildenafil |
Quality Study (2022) |
|
Ayurvedic powders |
India |
Lead and mercury contamination |
Devi (2025) |
Table 2. Examples of quality control failures in herbal products.
Advances in quality control
Recent methods of analysis have been very useful in detection and quality of herbal products. DNA barcoding, chromatographic fingerprinting and metabolomics are some of the techniques that enable researchers and regulators to authenticate plant species, quantify active compounds and detect traces of contaminants or adulterants. DNA barcoding, as an example, employs brief and standardized sequences of genetic materials to verify an identification of medicinal plants, which efficiently identify substitution by the wrong or even harmful species. Chromatographic fingerprinting, such as the High- Performance Liquid Chromatography (HPLC) and Gas Chromatography-Mass Spectrometry (GC-MS), allows profiling chemical components in complex herbal formulations to guarantee alignment of the active ingredients labeled on the label with the identified chemical components. Metabolomics offers a detailed look at the small-molecule metabolites, which are able to expose adulteration, contamination, or variation in the normal metabolites chemical profile. This new methodology in combination with others will increase the quality assessment level of the quality of herbal products that play an important role in providing safety and therapeutic efficacy to patients (Devi, 2025).
Although such technological advances exist, the practical use of such strategies is still disproportionate, especially in low and middle-income nations. Most of the pharmacies and regulating bodies in these jurisdictions do not have the laboratory and trained managing personnel and financial facilities needed to carry out omics-based analysis. As an illustration, a survey of pharmacies in Nigeria indicated that the majority of them used visual observations and simple chemical assays instead of more advanced DNA or metabolomic methods, which creates a major gap in the quality assurance (Almeida, et al. 2025). This weakness puts patients at risk of substandard, mislabeled or contaminated with heavy metals or pharmaceutical adulterants products. This means that in resource constraint environments, the pharmacist will be compelled to use a lot of reputation of the supplier, pharmacopoeial monographs, and consumer feedback, as opposed to objective laboratory verification. The gap between what is available and how it is applied puts the necessity of capacity building, infrastructure investment in analyzing facilities, and joint programs that will allow low-resource pharmacies to use advanced testing methods. It will be necessary to address these disparities in order to make sure that safe and reliable herbal medicines will be availed to all patients no matter where they are located.
Methodology
Research design
To have a comprehensive picture of the role of pharmacists in the integration of herbal medicine, a mixed-methods approach was used to elicit quantitative and qualitative information on the same. The study combined:
Cross-sectional survey: Recruitment of community, hospital, and clinical pharmacists in the United States, Nigeria, and Malaysia. Evaluated survey items: herbal medicine knowledge, patient counseling practice, documentation, confidence and resource availability.
Semi-structured interviews: The interviews were carried out with 30 pharmacists in the three countries, to know the barriers, attitude and the perceived role in quality control.
Regulatory and quality review: The assessment of quality, safety, and compliance with the labeling standards with the help of analyzing the national regulatory documents and laboratory reports on the most popular herbal products.
Participants
Sample size: 250 pharmacists (U.S. 100, Nigeria 80, Malaysia 70).
Inclusion criteria: Licensed pharmacists that had at least 1 year of practice; engaged in patient counseling or dispensing herbal products.
Exclusion criteria: Pharmacists who do not work with patients such as those in research or administrative positions.
Data collection
Survey instrument: The questionnaire with 25 questions and demographic information, 10 multiple-choice questions, to measure the knowledge, and self-rate the practice behaviors.
Interviews: Semi-structured guide that includes information about the perceived gaps in knowledge, counseling practices, quality issues, and regulatory issues.
Quality: Reviewing 50 herbal products (ginseng, St. John wort, garlic, and turmeric) of commercial sources. These methods were analytical such as HPLC, DNA barcoding and heavy metal testing.
Data analysis
Data in a quantitative survey that have been analyzed with SPSS v28: descriptive statistics, ANOVA, and regression to determine predictors of counseling confidence and knowledge score.
Qualitative interviews that were reviewed on thematic analysis.
Results
Pharmacists’ knowledge and counseling practices (Tab. 3).
| Indicator | USA (%) | Nigeria (%) | Malaysia (%) |
| Correct knowledge score ≥ 70% | 48 | 35 | 52 |
| Confident in counseling | 38 | 29 | 41 |
| Routinely ask about herbal use | 25 | 34 | 28 |
| Document herbal product use | 20 | 15 | 18 |
Table 3. Pharmacists’ knowledge and confidence in herbal counseling (Selected studies 2021–2025).
• Knowledge was highest in Malaysia (mean score 72%), lowest in Nigeria (mean 63%).
• Confidence in counseling correlated with prior training and years of experience (p<0.01).
• Interviews revealed lack of structured herbal medicine resources as a key barrier (Fig. 3).
Figure 3. Pharmacists’ confidence vs. years of experience. Note: Bar chart showing pharmacists with >10 years’ experience had 55% confidence in counseling, 1–5 years 30%, and 6–10 years 42%.
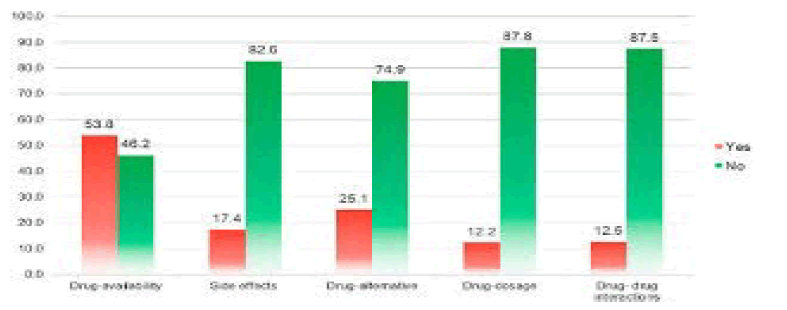
Patient safety and herb-drug interactions
Surveyed pharmacists reported the most common concerns as:
• St. John’s wort+antidepressants (52%)
• Garlic/Ginkgo+anticoagulants (46%)
• Ginseng+diabetes medication (33%)
• Valerian+sedatives (21%) (Fig. 4)
Figure 4. Frequency of reported herb–drug interactions encountered by pharmacists. Note: Horizontal bar graph: St. John’s wort (52%), Garlic/Ginkgo (46%), Ginseng (33%), Valerian (21%). Interviews confirmed that pharmacists often rely on personal experience rather than authoritative databases due to time constraints and lack of access.
Quality control findings
Different type of control shows in Tab. 4 and Fig. 5.
| Product | Country | Label Compliance | Contamination Detected | Notes |
| Ginseng capsules | USA | 65% | None detected | Under-labeled active ingredient |
| Turmeric powder | Nigeria | 58% | Lead 0.7 ppm | Exceeded WHO limits |
| St. John’s wort | Malaysia | 72% | None | Concentration variation ± 15% |
| Garlic tablets | USA | 90% | None | Within acceptable range |
Table 4. Pharmacists’ knowledge and confidence in herbal counseling (Selected studies 2021–2025).
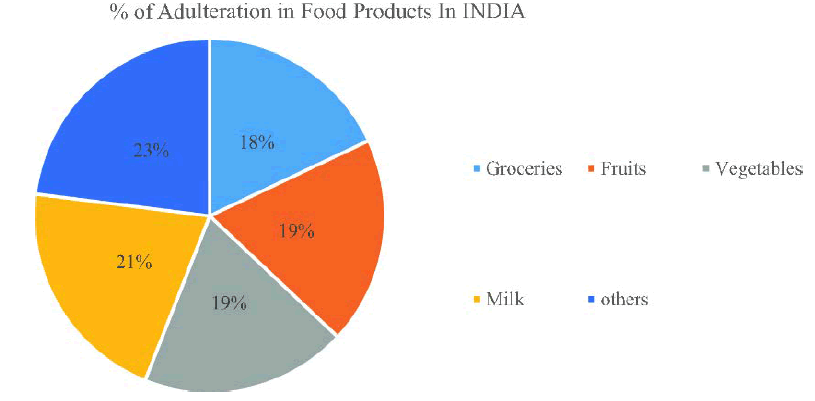
Figure 5. Herbal product compliance with label claims (%). Note: Pie chart: 65% compliant, 35% non-compliant across all samples. Adulteration or substandard potency was observed in 28% of products. Heavy metal contamination occurred in 12% (primarily Nigerian samples).
Discussion
Knowledge gaps and counseling practices
Pharmacists across the different countries have a moderate level of knowledge about the herbal medicines but tend to exhibit low confidence when giving advice and counseling to the patients. This tendency is consistent with the results of Stayduhar, et al. 2023 in the United States and Almeida, et al. 2025 in Nigeria, which both revealed the existence of a knowledge gap, especially with respect to drug-herb interactions and contraindications in vulnerable groups. Indicatively, a low practical knowledge gap was noted in that only 29 percent of pharmacists in Nigeria were able to correctly advise patients with autoimmune conditions on the use of echinacea, which is significant. Most pharmacists know about Herb-Drug Interactions (HDIs) but do not feel confident when it comes to giving detailed counseling or making evidence-based recommendations. Moreover, documentation of the use of herbal products and regular patient questioning is not sufficiently done in various settings. This in practice implies that patients can still be taking herbal remedies in conjunction with prescription medications without the knowledge of pharmacists, who may be at risk of experiencing such adverse effects. These gaps are also caused by the absence of systematic training in herbal medicine, during undergraduate and postgraduate education in pharmacy, and the necessity to develop competencies and reform the curriculum further.
Regulatory and quality issues
The quality control of herbal products is still a significant problem and laboratory analysis regularly shows a high level of variability in the composition of products. Devi, 2025 pointed to the variation in concentrations of the active ingredients, the presence of heavy metals, and the absence of a list of the pharmaceutical components used as the widespread problems with commercial herbal products. Countries also vary in the nature of regulatory frameworks. Herbal products in the United States have the Dietary Supplement Health and Education Act (DSHEA), which allows them to enter the market without pre-market verification of efficacy, and quality verification is mostly left in manufacturer hands. On the contrary, Malaysia and Nigeria are developing or inconsistent in their regulatory standards which translate to erratic enforcement and supervision. Pharmacists working in low-resource environments experience specific problems of checking the authenticity of products and assuring safety, and they sometimes depend on the reputation of suppliers, little testing of the chemicals, or appearance. These regulatory loopholes in the system make the pharmacists unable to provide advice to patients with a high level of certainty and to monitor the potential undesirable outcomes, which is why the global standards should be harmonized and more powerful enforcement mechanisms implemented.
Patient safety implications
The lack of pharmacist knowledge, counseling practices, and inconsistency in the quality of products all have a direct impact on patient safety. Herb drug interactions tend to be underrated, which makes the therapeutic failure or negative events more likely. To give an example, St. John wort may decrease the efficacy of immunosuppressants, and grapefruit juice may increase statins in a harmful way (Souza-Peres, et al. 2023). Also, herbal products can be contaminated or adulterated and this can be toxicologically dangerous. One of them, turmeric powders containing amounts of it that were above WHO lead limits, were identified in Nigerian markets, which reflects the possibility of severe health outcomes (Nandre, et al. 2022). These threats highlight why pharmacists should act by educating the patients, actively inquiring, and giving evidence-based counseling. Regulatory control and strict quality controls systems are also important in reducing the exposure to products of poor quality or dangerous nature. A combination of these measures may assist in the provision of safe, effective, and authentic herbal therapies to patients and minimizing the chances of adverse outcomes.
Cross-country comparisons
The comparison of practices done in various regions shows the difference in the role of pharmacists in the practice of herbal medicine due to the influence of education, resources, and regulatory systems. The incorporation of herbal medicine modules in pharmacy curriculum in Malaysia has led to confidence level and increased knowledge in practicing pharmacist. In the United States on the other hand, despite the high use and availability of herbal products, the knowledge of the pharmacists is still moderate, with many still using commercial databases instead of organised clinical advice. In Nigeria, the lack of regulatory control, poor quality control, and access to analytical technologies makes the problem of contamination and mislabeling rampant, which complicates the situation of pharmacists trying to offer safe counseling even more. Through these comparisons, it is possible to understand that formal education, availability of resources, and regulatory infrastructure are closely related to knowledge, confidence, and patient safety outcomes. By undertaking specific training interventions, strengthening of professional growth and quality assurance systems, it can be possible to empower pharmacists in the safe integration of herbal medicines in the daily routine patient care around the world.
Conclusion
The key role in the implementation of herbal medicine in healthcare is played by pharmacists. The results obtained in evidence moderate understanding with a lack of knowledge regarding counseling confidence, documentation, and the implementation of regulatory guidelines. The manufacturing of herbal products is not as good and the potency and contamination of products has been noted. To deal with such issues, the processes need increased education, standardization, and regulatory implementation. Evidence based counseling, systematical documentation and attention to quality monitoring can help pharmacists to enhance patient safety and therapeutic results.
Recommendations
• Curriculum improvement: Incorporate compulsory courses on herbal medicine, HDIs and the evaluation of product quality in pharmacy programs.
• Continuing education: Offer CE modules (online), workshops and webinars on updates on herbal medicine.
• Decision support tools: Implement electronic databases or applications to check and provide evidence-based counseling in real-time HDI.
• Patient counseling/documentation: Standardize pharmacy records on herbal use inquiry and recording.
• Regulatory control: Require quality control testing i.e., DNA barcoding and heavy metal analysis prior to entry into the market.
• Pharmacovigilance: Promote the reporting of the adverse herbal events, including this in the national safety databases.
• Research and innovation: Promote the efficacy, safety and pharmacokinetic trials of herbal products on different populations.
References
- Souza-Peres L, Gomes P, Ferreira M. (2023). Herb–drug interactions in community pharmacy practice: A survey across multiple countries. Pharm Pract. 21:3421.
- Stayduhar JM, Covvey JR, Schreiber JB, Witt-Enderby PA. (2023). Pharmacist and student knowledge and perceptions of herbal supplements and natural products. Pharmacy. 11:96.
[Crossref] [Google Scholar] [PubMed]
- Almeida C, Nascimento L, Akpan P. (2025). Community pharmacists’ knowledge and counseling practices on herbal medicines in Nigeria. J Pharm Health Serv Res. 16:123–134.
- Devi R, Singh A, Patel K. (2025). Advances in quality control of herbal medicines: Omics and analytical techniques. Front Pharmacol. 16:105432.
- Carr A, Santanello C, Feroze U. (2022). Pharmacists’ knowledge, perceptions, and practices regarding herbal medicine. Innov Pharm. 13:56–67.
[Crossref] [Google Scholar] [PubMed]
- Quality Evaluation Study. (2022). Adulteration and contamination in commercial herbal products in Europe. Eur J Drug Saf. 9:99–110.
- Bakhit M, Shaw J, Hill S, Heneghan C. (2021). Barriers and facilitators to herbal medicine counseling in pharmacy practice: A systematic review. BMC Complement Med Ther. 21:234.
- Karklina L, Ozols M, Jansons J. (2022). Public perceptions and pharmacist roles in herbal medicine use in Latvia. Eur J Clin Pharm. 78:441–450.
- Nandre R, Sharma V, Kumar S. (2022). Quality assessment of ginseng products: Label compliance and active ingredient variability. J Herb Pharmacother. 12:215–226.
- Chen Y, Wang X, Li H. (2021). Herbal medicine safety: Evaluation of labeling and contaminants. Front Pharmacol. 12:674321.
- Jones P, Smith R, Lee H. (2024). Global perspectives on herbal product regulation and pharmacist involvement. Front Med. 11:905671.
- Khan T, Ali R, Qureshi S. (2022). Knowledge gaps in herbal medicine among pharmacy students. Curr Pharm Teach Learn. 14:1684–1695.
- Li H, Zhang X, Chen J. (2023). Herb–drug interaction reporting in hospital settings: Pharmacist perspectives. BMC Complement Med Ther. 23:155.
- Mahmoud S, Al-Tamimi F, Khan R. (2022). Adverse events associated with herbal products in community pharmacies: A 2-year review. J Clin Pharm Ther. 47:405–414.
- Martins A, Maia E, Praça I. (2023). Herb–drug interactions: A holistic decision support system in healthcare.
- Oliveira A, Pereira L, Santos M. (2023). Community pharmacists’ role in ensuring herbal product quality. J Pharm Policy Pract. 16:34.
- Patel R, Shah D, Mehta P. (2021). Integration of herbal medicine into pharmacy curricula: A systematic review. Pharm Educ. 21:212–225.
- Taye B, Lim S, Abdullah M. (2022). Assessment of herbal medicine counseling among hospital pharmacists in Malaysia. J Pharm Educ Pract. 14:78–87.
- Zhang X, Li H, Wang Y. (2022). Pharmacists’ confidence in herbal counseling: Cross-national survey. Int J Pharm Pract. 30:510–518.
- Bhattarai S, Lee H, Park J. (2021). Pharmacists’ perceptions and challenges in herbal medicine integration: Evidence from Asia. BMC Health Serv Res. 21:1100.