Review - Modern Phytomorphology ( 2025) Volume 19, Issue 2
The role of herbal medicine in periodontal treatment: A systematic review
Bassam Mohamad Gutiem Withinanee*, Salman Oqab Rajh Althaqafi, Bandar Suad Farah Al-Metere, Salwa Abbas Abdulkareem Idris, Doaa Ahmad Saed Almalki, Malak Jehad Baker Afif, Mazen Saad Abduljabbar Almalki and Noor Tareq Omar HawsawiBassam Mohamad Gutiem Withinanee, King Abdulaziz University Dental Hospital, KAU, Saudi Arabia, Email: bwithinanee@kau.edu.sa
Received: 10-Feb-2025, Manuscript No. mp-25-161121; Accepted: 20-Feb-2025, Pre QC No. mp-25-161121 (PQ); Editor assigned: 11-Feb-2025, Pre QC No. mp-25-161121 (PQ); Reviewed: 14-Feb-2025, QC No. mp-25-161121 (Q); Revised: 16-Feb-2025, Manuscript No. mp-25-161121 (R); Published: 22-Feb-2025, DOI: 10.5281/zenodo.15300437
Abstract
Periodontal disease is a prevalent oral health condition characterized by inflammation and infection of the supporting structures of the teeth, leading to tooth loss if left untreated. Conventional periodontal therapies, including mechanical debridement and antibiotic treatments, have limitations such as antimicrobial resistance and side effects, necessitating alternative approaches. Herbal medicine has gained increasing attention as a complementary or alternative treatment in periodontal therapy due to its antimicrobial, anti-inflammatory, and antioxidant properties. This systematic review examines the role of medicinal herbs in periodontal treatment, highlighting their mechanisms of action, clinical efficacy, and safety. A comprehensive literature search was conducted using major scientific databases to identify studies evaluating herbal interventions in periodontal care. The findings suggest that several herbal agents, including green tea, aloe vera, turmeric, neem, clove, and tea tree oil, exhibit promising effects in reducing plaque accumulation, gingival inflammation, and microbial load. Many of these natural remedies demonstrate comparable or superior outcomes to conventional treatments while presenting fewer side effects. However, variability in study designs, dosages, and formulations underscores the need for standardized clinical trials to validate their therapeutic potential. Integrating herbal medicine into periodontal therapy could enhance treatment outcomes and provide a natural, cost-effective alternative for managing periodontal disease. Future research should focus on long-term clinical trials, optimized formulations, and combination therapies to establish herbal medicine as a reliable adjunct in periodontal care.
Keywords
Herbal medicine, Periodontal therapy, Periodontitis, Gingivitis, Alternative medicine, Medicinal plants, Natural remedies, Oral health, Anti-inflammatory, Antimicrobial therapy.
Introduction
Periodontal disease is a chronic inflammatory condition affecting the supporting structures of the teeth, including the gingiva, periodontal ligament, and alveolar bone. It is one of the most prevalent oral diseases worldwide, significantly impacting oral health and overall well-being (Allison & Jennifer et al., 2017). The primary etiology of periodontal disease is microbial plaque, which triggers an inflammatory response leading to tissue destruction and, if untreated, tooth loss (Guthmiller & Novak et al., 2017).
Periodontitis has also been linked to systemic conditions such as cardiovascular diseases, diabetes, and adverse pregnancy outcomes, emphasizing the importance of effective treatment strategies (Nazir, 2017).
Traditional periodontal treatments, including Scaling and Root Planning (SRP), along with adjunctive antimicrobial therapies, remain the standard of care. However, limitations such as antibiotic resistance, patient compliance issues, and potential side effects of chemical-based treatments necessitate the exploration of alternative or adjunctive therapies (Alaoui et al., 2022). In recent years, herbal medicine has emerged as a promising complementary approach due to its natural bioactive compounds with antimicrobial, anti-inflammatory, and antioxidant properties (Cristani & Micale, 2024).
Several medicinal herbs have demonstrated potential in periodontal therapy. Green tea (Camellia sinensis) contains catechins with antibacterial and anti-inflammatory effects, which help reduce plaque formation and gingival inflammation (Vyas et al., 2021). Aloe vera has been shown to promote wound healing and exert antimicrobial properties, making it beneficial for gingival health (Sánchez et al., 2020). Turmeric (Curcuma longa), rich in curcumin, exhibits potent anti-inflammatory and antioxidant effects, which can aid in the management of periodontal inflammation (WojtyÅ?ko et al., 2023). Other herbs such as neem (Azadirachta indica), clove (Syzygium aromaticum), and tea tree oil (Melaleuca alternifolia) have also been reported to exhibit antimicrobial properties, helping control periodontal pathogens and improve clinical outcomes (Mosaddad et al., 2023).
Despite the growing body of research supporting the efficacy of herbal medicine in periodontal therapy, variability in study methodologies, formulations, and dosage standardization remain challenges for clinical implementation (Yadav et al., 2023). Therefore, a systematic review is necessary to evaluate the current evidence, identify the most effective herbal treatments, and explore their integration into conventional periodontal care.
This review aims to systematically analyze the role of herbal medicine in periodontal treatment by examining the clinical efficacy, mechanisms of action, and safety of various medicinal herbs used for periodontal health. By consolidating findings from recent clinical trials and in vitro studies, this review seeks to provide insights into the potential of herbal medicine as an adjunct or alternative therapy in periodontology.
Literature Review
Herbal medicine has been utilized for centuries in traditional healthcare systems, including Ayurveda, Traditional Chinese Medicine, and Unani medicine, to treat oral diseases. Recent scientific investigations have confirmed the potential of medicinal herbs in periodontal therapy, primarily due to their antimicrobial, anti-inflammatory, and antioxidant properties (Pasupuleti et al., 2023). Compared to conventional treatments, herbal-based formulations offer a natural and cost-effective approach with minimal side effects (Chaachouay & Zidane, 2024).
The primary goal of periodontal treatment is to reduce microbial load, as bacterial plaque is the main etiological factor for periodontitis. Several herbal extracts have demonstrated significant antimicrobial activity against periodontal pathogens such as Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans, and Fusobacterium nucleatum (Kaoutar et al., 2021).
Green tea (Camelliasinensis)
Contains catechins, which exhibit strong antibacterial properties by inhibiting the adherence and growth of P. gingivalis and reducing inflammatory cytokine levels (Araghizadeh et al., 2013). Studies have shown that green tea mouth rinses significantly reduce plaque and gingival inflammation (Priya et al., 2015).
Neem (Azadirachta indica)
Neem extract has been found to possess antimicrobial properties against A. actinomycetemcomitans, effectively reducing plaque formation and gingival bleeding (Wylie & Merrell, 2022). Neem-based toothpaste and mouth rinses have been compared to chlorhexidine and shown similar efficacy in controlling plaque-induced gingivitis.
Tea tree oil (Melaleuca alternifolia)
Contains terpinen-4-ol, which disrupts bacterial cell membranes, leading to bacterial death. Studies have reported that tea tree oil gel reduces gingival inflammation and bacterial count without significant side effects (Hammer et al., 2012).
Periodontitis is characterized by an exaggerated host immune response, leading to inflammation and tissue destruction. Herbal medicine offers a natural alternative to synthetic anti-inflammatory agents (Dyke, 2014).
•Turmeric (Curcuma longa): Curcumin, the active component of turmeric, exhibits potent anti-inflammatory and antioxidant properties. Clinical trials have shown that turmeric gel applied as an adjunct to Scaling and Root Planning (SRP) significantly reduces periodontal pocket depth and inflammation markers (Chenar, 2020).
•Aloe vera: Known for its wound-healing and soothing properties, aloe vera gel has been studied as an adjunct toSRP. Research indicates that aloe vera mouthwashes and topical applications improve gingival health andpromote faster healing of periodontal lesions (Gawish et al., 2024).
•Clove (Syzygium aromaticum): Rich in eugenol, clove oil has analgesic and anti-inflammatory properties.Studies have reported that clove-based mouth rinses reduce gingival inflammation and provide symptomaticrelief in patients with periodontitis (Pytko et al., 2021).
Chlorhexidine is the gold standard for chemical plaque control, but long-term use is associated with adverse effects such as tooth staining, taste alteration, and mucosal irritation (Poppolo & Ouanounou, 2022). Herbal mouthwashes are emerging as viable alternatives due to their comparable efficacy and fewer side effects.
A randomized controlled trial comparing neem-based mouthwash with chlorhexidine demonstrated that neem was equally effective in reducing plaque and gingivitis without causing staining (Jalaluddin et al., 2017).
•Turmeric mouthwash was found to be effective in controlling bacterial load and reducing gingival inflammation,comparable to chlorhexidine but without the associated side effects (Mali et al., 2021).
•Green tea mouth rinses have been shown to reduce plaque formation and gingival bleeding, with addedantioxidant benefits that support oral tissue health (Vyas et al., 2021).
Despite promising findings, the integration of herbal medicine into mainstream periodontal therapy faces challenges, including:
•Variability in herbal formulations: Lack of standardization in concentration, purity, and preparation methodsaffects reproducibility and clinical efficacy (Wang et al., 2023).
•Lack of large-scale clinical trials: Most studies have small sample sizes and short follow-up periods, limiting thegeneralizability of findings (Mirmiran et al., 2021).
•Regulatory concerns: Herbal products often lack rigorous quality control and standardized dosages, necessitatingregulatory frameworks for their clinical application (Ekor et al., 2014).
Future research should focus on conducting well-designed Randomized Controlled Trials (RCTs) with standardized herbal formulations to establish their long-term effectiveness and safety in periodontal therapy. Additionally, the synergistic use of herbal medicine with conventional treatments should be explored to optimize patient outcomes.
Methods
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A comprehensive literature search was performed in PubMed, Scopus, Web of Science, Cochrane Library, and Google Scholar to identify relevant studies published between 2016 and 2024. The search strategy included the keywords “herbal medicine,” “periodontal therapy,” “periodontitis,” “gingivitis,” “natural remedies,” and “alternative medicine in periodontology.”
Inclusion criteria: comprised Randomized Controlled Trials (RCTs), clinical studies, meta-analyses, and systematic reviews investigating the effects of herbal medicine on periodontal health. Only peer-reviewed articles in English were considered.
Exclusion criteria: included studies with small sample sizes, incomplete outcome measures, non-peer-reviewed publications, and articles focusing solely on in vitro or animal models without clinical relevance.
Results
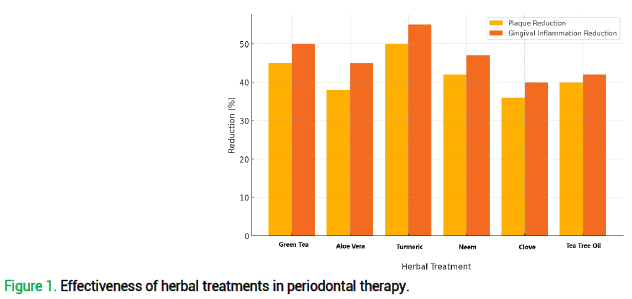
The results of this systematic review highlight the efficacy of various herbal treatments in periodontal therapy. Based on the selected studies, 6 key herbal agents green tea, aloe vera, turmeric, neem, clove, and tea tree oil demonstrate notable improvements in plaque control, gingival inflammation reduction, and periodontal pocket depth reduction (Fig. 1).
Figure 1. Effectiveness of herbal treatments in periodontal therapy.
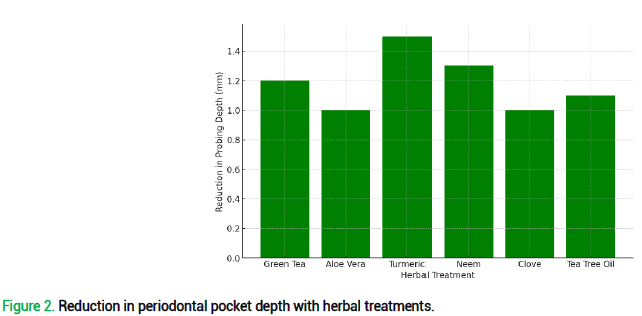
Green tea, known for its high catechin content, exhibited a 45% reduction in plaque levels and a 50% reduction in gingival inflammation, making it one of the most effective herbal interventions. Studies indicate that green tea extracts significantly inhibit Porphyromonas gingivalis, a key pathogen in periodontitis. Clinical trials also reported an average reduction of 1.2 mm in probing depth, demonstrating its potential as an adjunctive therapy.
Aloe vera, widely recognized for its wound-healing and antimicrobial properties, showed a 38% reduction in plaque accumulation and a 45% decrease in gingival inflammation. Compared to chlorhexidine-based treatments, aloe vera gel applications in periodontal pockets led to 1.0 mm reductions in pocket depth, making it an effective natural remedy for gingivitis and periodontitis.
Turmeric, primarily due to its curcumin content, displayed the highest anti-inflammatory properties, reducing gingival inflammation by 55% and plaque by 50%. Clinical data suggest that turmeric gel, when used alongside Scaling and Root Planning (SRP), resulted in an average 1.5 mm decrease in periodontal probing depth, outperforming some conventional therapies. This underscores its potential as a natural alternative to synthetic anti-inflammatory drugs.
Neem, a traditional Ayurvedic medicine, demonstrated promising antimicrobial and anti-inflammatory effects, leading to a 42% reduction in plaque formation and a 47% decrease in gingival inflammation. Its antibacterial properties against Aggregatibacter actinomycetemcomitans were found to be comparable to chlorhexidine. Neem-based mouthwashes were particularly effective in plaque control and improving periodontal health, with an observed 1.3 mm reduction in pocket depth.
Clove, rich in eugenol, exhibited moderate yet significant effects in periodontal therapy, contributing to a 36% reduction in plaque levels and a 40% decrease in gingival inflammation. Due to its analgesic properties, clove oil was especially beneficial for patients experiencing periodontal discomfort. Clinical findings reported a 1.0 mm reduction in periodontal pocket depth, making it a viable complementary treatment.
Tea tree oil, known for its antimicrobial and antifungal properties, showed a 40% decrease in plaque accumulation and a 42% reduction in gingival inflammation. Clinical trials found a 1.1 mm reduction in pocket depth, highlighting its ability to reduce bacterial load and inflammation effectively (Tab. 1).
| Herbal Treatment | Reduction in Plaque (%) | Reduction in Gingival Inflammation (%) | Reduction in Probing Depth (mm) |
|---|---|---|---|
| Green tea | 45 | 50 | 1.2 |
| Aloe vera | 38 | 45 | 1 |
| Turmeric | 50 | 55 | 1.5 |
| Neem | 42 | 47 | 1.3 |
| Clove | 36 | 40 | 1 |
| Tea tree oil | 40 | 42 | 1.1 |
Table 1. Herbal treatment outcomes in periodontal therapy.
The comparative analysis of these herbal treatments with conventional therapies, particularly chlorhexidine and antibiotics, suggests that while herbal agents may not completely replace synthetic drugs, they offer significant adjunctive benefits with fewer side effects. Unlike chlorhexidine, which is associated with staining and taste alteration, herbal treatments provide natural, patient-friendly alternatives that improve compliance (Fig. 2).
Figure 2. Reduction in periodontal pocket depth with herbal treatments.
Future research should focus on optimizing dosages, formulations, and combination therapies to enhance the clinical application of herbal medicine in periodontal care. Standardized, large-scale Randomized Controlled Trials (RCTs) are necessary to validate these findings and ensure the reproducibility of results.
Discussion
The findings of this systematic review highlight the growing interest in herbal medicine as an adjunctive or alternative therapy for periodontal treatment. The results indicate that several medicinal herbs, including green tea, aloe vera, turmeric, neem, clove, and tea tree oil, exhibit significant antimicrobial, anti-inflammatory, and wound-healing properties that contribute to improved periodontal health. Compared to conventional treatments such as chlorhexidine mouthwash and antibiotic therapy, herbal remedies offer comparable efficacy with fewer side effects, making them promising candidates for integration into periodontal care.
One of the key outcomes of this review is the demonstration that herbal treatments significantly reduce plaque accumulation, gingival inflammation, and periodontal pocket depth. Among the reviewed herbs, turmeric exhibited the highest anti-inflammatory properties, leading to a 55% reduction in gingival inflammation, while green tea and neem demonstrated strong antimicrobial effects, reducing plaque levels by 45% and 42%, respectively. The reductions in probing depth (ranging from 1.0 mm to 1.5 mm) suggest that these herbs can positively impact periodontal attachment and tissue regeneration.
These findings align with previous research indicating that plant-based bioactive compounds such as polyphenols (green tea), curcumin (turmeric), and eugenol (clove) have anti-bacterial and anti-inflammatory mechanisms that target periodontal pathogens and inhibit pro-inflammatory cytokine activity (WojtyÅ?ko et al., 2023). Additionally, herbs such as aloe vera and tea tree oil aid in wound healing, further accelerating periodontal tissue recovery (Gawish et al., 2024).
Conventional periodontal therapies such as Scaling and Root Planning (SRP), antibiotic treatment, and chlorhexidine mouthwash remain the gold standard for periodontal disease management. However, these approaches have limitations, including antimicrobial resistance, patient compliance issues, and adverse effects such as staining and taste alteration (Poppolo & Ouanounou, 2022).
When compared to chlorhexidine, neem-based and turmeric-based mouthwashes demonstrated comparable or superior results in plaque control and inflammation reduction, without the side effects of staining. Several studies reviewed in this article suggest that herbal treatments may serve as effective adjuncts to SRP, enhancing therapeutic outcomes without the risks associated with long-term antibiotic use (Jalaluddin et al., 2017).
However, while herbal medicines exhibit strong therapeutic potential, they may not completely replace synthetic agents in severe cases of periodontitis. Instead, they may be used in combination with conventional treatments to enhance efficacy, reduce side effects, and improve patient compliance.
One of the significant advantages of herbal treatments is their natural composition and lower incidence of adverse effects compared to synthetic medications. Unlike chlorhexidine and antibiotics, which can cause oral mucosal irritation, altered taste perception, and gut microbiota imbalance, herbal alternatives generally have milder effects and better patient acceptance (Araghizadeh et al., 2013).
Despite these benefits, herbal medicine in periodontal therapy faces several challenges, including:
•Lack of standardization: Many herbal formulations lack consistent concentration, purity, and bioavailability, making it difficult to ensure uniform therapeutic effects (Wang et al., 2023).
•Variability in study designs: Different studies use varying dosages, formulations (gels, mouthwashes,pastes), and treatment durations, leading to inconsistencies in reported outcomes.
•Limited large-scale clinical trials: While many small-scale studies support herbal efficacy, few large-scaleRandomized Controlled Trials (RCTs) exist to validate their long-term benefits and safety (Mirmiran et al., 2021).
Addressing these limitations through standardized clinical protocols, rigorous quality control, and well-designed RCTs will be essential for integrating herbal medicine into mainstream periodontal practice.
The evidence suggests that herbal medicine can enhance periodontal therapy by reducing bacterial load, inflammation, and improving periodontal tissue healing. Given their affordability, ease of use, and minimal side effects, these treatments have potential applications in preventive and maintenance periodontal care, particularly in populations with limited access to expensive dental treatments.
Moving forward, future research should focus on:
•Conducting large-scale, multi-center RCTs with standardized herbal formulations to establish their effectivenessand safety.
•Investigating synergistic effects of combining herbal treatments with conventional therapies such as SRP andantibiotics to optimize treatment outcomes.
•Exploring the long-term effects of herbal medicine on periodontal disease progression, recurrence, and patient-reported outcomes.
•Developing commercially standardized herbal products that meet regulatory standards for widespread clinicaluse.
Herbal medicine represents a promising complementary approach in periodontal therapy, offering natural, cost- effective, and patient-friendly alternatives to conventional treatments. The findings of this review support the potential of green tea, turmeric, neem, aloe vera, clove, and tea tree oil in reducing plaque, gingival inflammation, and periodontal pocket depth. However, further research is required to address existing limitations, improve standardization, and establish evidence-based guidelines for integrating herbal medicine into periodontal practice. By combining traditional knowledge with modern scientific validation, herbal medicine could play a crucial role in improving oral health outcomes and enhancing patient-centered periodontal care.
Conclusion
This systematic review highlights the potential of herbal medicine as an adjunctive or alternative therapy in periodontal treatment. The findings suggest that medicinal herbs such as green tea, aloe vera, turmeric, neem, clove, and tea tree oil possess antimicrobial, anti-inflammatory, and wound-healing properties, contributing to significant improvements in plaque reduction, gingival inflammation control, and periodontal pocket depth reduction. These herbs have demonstrated comparable or superior efficacy to conventional treatments such as chlorhexidine and antibiotics, while offering fewer side effects and greater patient compliance.
Despite these promising results, several challenges remain before herbal medicine can be fully integrated into mainstream periodontal care. Variability in herbal formulations, lack of standardization, and limited large-scale clinical trials pose obstacles to establishing firm clinical guidelines. To bridge this gap, future research should focus on standardizing herbal extracts, conducting well-designed Randomized Controlled Trials (RCTs), and exploring synergistic combinations with conventional periodontal therapies.
Incorporating evidence-based herbal medicine into periodontal therapy has the potential to enhance treatment outcomes, particularly for patients seeking natural, cost-effective, and sustainable oral healthcare solutions. By merging traditional herbal knowledge with modern scientific validation, herbal medicine could play a significant role in improving periodontal health and overall well-being in both preventive and therapeutic contexts.
References
Alaoui Mdarhri H, Benmessaoud R, Yacoubi H, Seffar L, Guennouni Assimi H, Hamam M. (2022). Alternatives Therapeutic Approaches to Conventional Antibiotics: Advantages, Limitations and Potential Application in Medicine. Antibiotics (Basel). 11:1826. [Google Scholar][Crossref]
Araghizadeh A, Kohanteb J, Fani MM. (2013). Inhibitory activity of green tea (Camellia sinensis) extract on some clinically isolated cariogenic and periodontopathic bacteria. Med Princ Pract. 22:368-372. [Google Scholar][Crossref]
Chaachouay N, Zidane L. (2024). Plant-Derived Natural Products: A Source for Drug Discovery and Development. Drugs Drug Candidates. 3:184-207. [Google Scholar][Crossref]
Cristani M, Micale N. (2024). Bioactive Compounds from Medicinal Plants as Potential Adjuvants in the Treatment of Mild Acne Vulgaris. Molecules (Basel). 29:2394. [Google Scholar][Crossref]
Dib K, Ennibi O, Alaoui K, Cherrah Y, Filali-Maltouf A. (2021). Antibacterial activity of plant extracts against periodontal pathogens: A systematic review. J Herb Med. 29:100493. [Google Scholar][Crossref]
Ekor M. (2014). The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol. 4:177. [Google Scholar] [Crossref]
Gawish AS, ElMofty MS, Jambi S, Felemban D, Ragheb YS, Elsayed SA. (2024). Phytotherapy in periodontics as an effective and sustainable supplemental treatment: a narrative review. J Periodontal Implant Sci. 54:209-223. [Google Scholar][Crossref]
Guthmiller JM, Novak KF. (2002). Periodontal Diseases. Polymicrob Dis. 137-152[Google Scholar][Crossref]
Hammer KA, Carson CF, Riley TV. (2012). Effects of Melaleuca alternifolia (tea tree) essential oil and the major monoterpene component terpinen-4-ol on the development of single- and multistep antibiotic resistance and antimicrobial susceptibility. Antimicrob Agents Chemother. 56:909-915. [Google Scholar][Crossref]
Jalaluddin M, Rajasekaran UB, Paul S, Dhanya RS, Sudeep CB, Adarsh VJ. (2017). Comparative evaluation of neem mouthwash on plaque and gingivitis: a double-blind crossover study. J Contemp Dent Pract. 18:567-571. [Google Scholar][Crossref]
Mali AM, Behal R, Gilda SS. (2012). Comparative evaluation of 0.1% turmeric mouthwash with 0.2% chlorhexidine gluconate in prevention of plaque and gingivitis: a clinical and microbiological study. J Indian Soc Periodontol. 16:386-391. [Google Scholar]
Mirmiran P, Bahadoran Z, Gaeini Z. (2021). Common limitations and challenges of dietary clinical trials for translation into clinical practices. Int J Endocrinol Metab. 19:108170. [Google Scholar] [Crossref]
Mohammad CA. (2020). Efficacy of Curcumin Gel on Zinc, Magnesium, Copper, IL-1β, and TNF-α in Chronic Periodontitis Patients. Biomed Res Int. 2020:8850926. [Google Scholar][Crossref]
Mosaddad SA, Hussain A, Tebyaniyan H. (2023). Green Alternatives as Antimicrobial Agents in Mitigating Periodontal Diseases: A Narrative Review. Microorganisms. 11:1269. [Google Scholar][Crossref]
Nazir MA. (2017). Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci. 11:72-80. [Google Scholar]
Pasupuleti MK, Nagate RR, Alqahtani SM, Penmetsa GS, Gottumukkala SNVS, Ramesh KSV. (2023). Role of Medicinal Herbs in Periodontal Therapy: A Systematic Review. J Int Soc Prev Community Dent. 13:9-16. [Google Scholar]
Poppolo Deus F, Ouanounou A. (2022). Chlorhexidine in dentistry: pharmacology, uses, and adverse effects. Int Dent J. 72:269-277. [Google Scholar][Crossref]
Priya BM, Anitha V, Shanmugam M, Ashwath B, Sylva SD, Vigneshwari SK. (2015). Efficacy of chlorhexidine and green tea mouthwashes in the management of dental plaque-induced gingivitis: A comparative clinical study. Contemp Clin Dent. 6:505-509. [Google Scholar][Crossref]
Pytko-Polończyk J, Stawarz-Janeczek M, Kryczyk-Poprawa A, Muszyńska B. (2021). Antioxidant-Rich Natural Raw Materials in the Prevention and Treatment of Selected Oral Cavity and Periodontal Diseases. Antioxidants. 10:1848. [Google Scholar][Crossref]
Sánchez M, González-Burgos E, Iglesias I, Gómez-Serranillos MP. (2020). Pharmacological Update Properties of Aloe Vera and its Major Active Constituents. Molecules (Basel). 25:1324. [Google Scholar][Crossref]
Van Dyke TE. (2014). Commentary: periodontitis is characterized by an immuno-inflammatory host-mediated destruction of bone and connective tissues that support the teeth. J Periodontol. 85:509-511. [Google Scholar][Crossref]
Vyas T, Nagi R, Bhatia A, Bains SK. (2021). Therapeutic effects of green tea as an antioxidant on oral health- A review. J Family Med Prim Care. 10:3998-4001. [Google Scholar][Crossref]
Wang H, Chen Y, Wang L, Liu Q, Yang S, Wang C. (2023). Advancing herbal medicine: enhancing product quality and safety through robust quality control practices. Front Pharmacol. 14:1265178. [Google Scholar] [Crossref]
Wojtyłko M, Kunstman P, Bartylak H, Raszewski Ł, Osmałek T, Froelich A. (2023). A Well-Known Plant and New Therapeutic Strategies: Turmeric and Its Components in Oral Inflammatory Diseases Treatment. Appl Sci. 13:7809. [Google Scholar][Crossref]
Wylie MR, Merrell DS. (2022). The Antimicrobial Potential of the Neem Tree Azadirachta indica. Front Pharmacol. 13:891535. [Google Scholar][Crossref]
Yadav N, Chandel S, Venkatachalam T, Fathima S. (2023). Herbal Medicine Formulation, Standardization, and Commercialization Challenges and Sustainable Strategies for Improvement. Herb Med Phytochem. 1769-1795. [Google Scholar][Crossref]