Review Article - Modern Phytomorphology ( 2025) Volume 19, Issue 6
Pharmacists’ knowledge, attitudes and practices toward herbal medicine: An integrative review
Hassan Muslih Alraddadi1*, Muhannad Ghali Alenezi1, Ziyad Jameel Alrehaili1, Abdullah Mossaed Alahmadi1, Mohammed Faisal Alyanbaawe1, Rayan Mohammed Alharbi1, Fayez Jabal Alshahrani1 and Abdulaziz Ijl Alrehaili22National Guard Health Affairs, Yanbu, Saudi Arabia
Hassan Muslih Alraddadi, National Guard Health Affairs, Madina, Saudi Arabia, Email: alraddadiha@mngha.med.sa
Received: 22-Aug-2025, Manuscript No. mp-25-171491 ; , Pre QC No. mp-25-171491 (PQ); Editor assigned: 25-Aug-2025, Pre QC No. mp-25-171491 (PQ); Reviewed: 01-Sep-2025, QC No. mp-25-171491 ; Revised: 05-Oct-2025, Manuscript No. mp-25-171491 (R); Published: 11-Oct-2025, DOI: 10.5281/zenodo.17983289
Abstract
Herbal medicine is increasingly used worldwide as an alternative and complementary therapy. Pharmacists, as frontline healthcare professionals, play a pivotal role in guiding patients on the safe and effective use of herbal products. However, variations in their Knowledge, Attitudes, and Practices (KAP) remain a challenge for integrating herbal medicine into modern healthcare. This review synthesizes global evidence on pharmacists’ KAP toward herbal medicine, highlighting regional differences, key barriers, and opportunities for strengthening pharmacists’ role. Findings indicate that while pharmacists generally recognize the potential value of herbal medicine, their knowledge is often insufficient, attitudes vary from supportive to skeptical, and practices are hindered by limited training, regulation, and evidence-based guidelines. Addressing these gaps requires targeted education, standardized regulations, and improved pharmacist–patient communication.
Keywords
Herbal medicine, Pharmacists, Knowledge, attitudes, Practices, Integrative review, Patient counseling
Introduction
Herbal medicine remains one of the most widely practiced therapeutic modalities, and its effective use depends on accurate recognition and evaluation of plant-derived materials. Modern phytomorphology is the study of plant structural characteristics supports the authentication of medicinal plants by examining leaf patterns, stem anatomy, reproductive structures, and microscopic features such as trichomes or stomatal architecture. These characteristics help distinguish genuine medicinal plants from adulterants, which is essential for maintaining the safety and therapeutic value of herbal preparations (Miranda, 2021). Pharmacists, as primary dispensers of herbal products, must be familiar with the morphological traits that influence quality control, storage, and selection of plant-based remedies. Despite this need, many pharmacists receive limited formal training in plant morphology, contributing to gaps in their knowledge, confidence, and counseling practices (For example: asparagus, celery) (Wachtel-Galor and Benzie, 2011).
Despite their widespread use, herbal medicines are not without risks. Studies highlight potential herb-drug interactions, quality control challenges, and uncertainties regarding safety and efficacy (Brantley, et al. 2014). These concerns emphasize the need for professional oversight in the use of herbal products. Pharmacists, as the most accessible healthcare providers, are in a unique position to guide patients on the appropriate, safe, and effective use of herbal medicines (Ng, et al. 2021).
Pharmacists' roles extend beyond dispensing; they are responsible for patient education, pharmacovigilance, and ensuring therapeutic outcomes. However, evidence suggests their knowledge of herbal medicines is inconsistent, attitudes range from supportive to skeptical, and their practices often fall short of patient expectations (Zaidi, et al. 2022, Khdour, et al. 2018). In many regions, pharmacy curricula lack adequate training in herbal pharmacology, leaving pharmacists underprepared to meet patient demand (Al-Jedai, et al. 2016).
The importance of investigating pharmacists''Knowledge, Attitudes, and Practices (KAP) toward herbal medicine is underscored by the global rise in herbal product consumption. Understanding pharmacists perspectives can provide insight into existing gaps, identify barriers to effective practice, and inform strategies to enhance their role in herbal medicine counseling. This integrative review aims to synthesize current evidence on pharmacists KAP regarding herbal medicine, highlight regional variations, and propose recommendations for strengthening pharmacists, contribution to safe and effective herbal medicine use.
Methodology
The inclusion criteria required studies to be focused on pharmacists in community or hospital settings, exploring knowledge, attitudes, or practices toward herbal medicines, based on original research (quantitative, qualitative, or mixed methods) and published in peer-reviewed journals. Excluded were studies examining other healthcare professionals (physicians, nurses), patient-only surveys, review articles, conference abstracts without full data, and studies focusing solely on non-herbal dietary supplements.
This integrative review followed a structured approach to gather and synthesize studies on pharmacists’ knowledge, attitudes, and practices toward herbal medicine (For example: ginger for nausea, garlic for heart health, St. John’s Wort for depression, and valerian root for sleep). Although the primary focus was KAP, this revised version acknowledges that many studies indirectly relate to phytomorphology when discussing plant authentication, source reliability, and quality control of herbal materials. A comprehensive search was performed in PubMed, Scopus, Web of Science, and Google Scholar. Studies published between 2000 and 2025 were included, focusing on pharmacists in hospital and community settings. Findings were classified by region to highlight contextual differences in training quality, regulatory frameworks, and access to plant identification resources.
Allincluded studies wereimported into EndNotefororganization,and duplicateswereremoved.Twoindependent reviewers extracted key data, which included the author(s), year of publication, country or region, study design, sample size, type of practice setting, and primary findings across the domains of knowledge, attitudes, and practices. Discrepancies in data extraction were resolved through discussion until consensus was achieved.
To enable meaningful comparison, the included studies were categorized according to geographic region: Europe, North America, Middle East, Asia, and Africa. This categorization reflects variations in pharmacy education, regulatory frameworks, and cultural reliance on herbal medicine, thereby allowing analysis of contextual influences on pharmacists’ KAP. Within each region, studies were compared in terms of methodological rigor, sample composition, and reported findings.
The Mixed Methods Appraisal Tool (MMAT, 2018) was used to assess study quality. Quantitative surveys were examined for sampling strategy, response rate, and validity of instruments. Qualitative studies were appraised for clarity of research questions, adequacy of data collection, and credibility of analysis. Mixed-methods designs were evaluated for coherence between quantitative and qualitative components. Studies that scored low in methodological quality were not excluded but were discussed with caution, particularly when their findings deviated substantially from higher-quality studies.
Thematic synthesis was employed to analyze findings across studies. First, results were summarized for each region in terms of knowledge, attitudes, and practices. These findings were then compared across regions to identify similarities and divergences. Quantitative data, such as percentages of pharmacists with adequate knowledge or positive attitudes, were tabulated for clarity. Qualitative insights, including themes about barriers or professional concerns, were integrated to complement numerical trends.
To illustrate regional differences, two tables were developed. Tab. 1 synthesizes pharmacists’ knowledge, attitudes, and practices across regions, alongside reported barriers to effective engagement with herbal medicine. These tables were designed to allow cross-study comparison and highlight areas where pharmacists demonstrate strengths or weaknesses.
| Region | Knowledge Level | Attitudes | Practices | Reported Barriers |
| Middle East | Low–moderate; weak in herb–drug interactions | Generally positive | Limited to dispensing | Lack of training; poor regulations |
| Europe | Moderate; better formal training | Cautious, evidence-driven | Counseling when evidence available | Safety concerns; liability issues |
| Asia | Low–moderate; inconsistent curricula | Positive, patient-centered | Minimal proactive counseling | Lack of evidence-based guidelines |
| North America | Moderate; awareness of herb–drug risks | Mixed, often skeptical | Counseling only upon request | Concerns over efficacy and regulation |
| Africa | Low; limited formal education | Mixed, often uncertain | Minimal counseling | Dominance of traditional healers; weak regulation |
Table 1. Comparative analysis of pharmacists’ knowledge, attitudes, and practices by region.
The integrative approach was chosen because it allowed for inclusion of both quantitative survey data and qualitative insights, offering a richer understanding of pharmacists’ KAP. Dividing the samples into regions made it possible to contextualize pharmacists’ perspectives within their cultural and regulatory environments. Without such a comparative approach, the interpretation of findings would be fragmented and fail to capture the influence of systemic and educational factors.
Furthermore, by synthesizing evidence into comparative tables, this methodology ensures clarity in demonstrating both global patterns and regional nuances. For example, while pharmacists in Europe and North America report more cautious attitudes due to safety concerns, those in Asia and the Middle East exhibit positive attitudes but limited practical application, often constrained by weak training and regulation. In Africa, the interaction between formal pharmacy practice and traditional medicine systems creates unique barriers that are less evident elsewhere.
Results
Across regions, pharmacists demonstrated varying levels of knowledge regarding herbal medicine, with notable gaps concerning plant identification and the morphological characteristics essential for distinguishing authentic herbal raw materials. While some pharmacists recognized major medicinal plant families (Which includes Asteraceae (e.g., chamomile, echinacea), Lamiaceae (e.g., mint, basil, rosemary), Solanaceae (e.g., ashwagandha, nightshade), and Zingiberaceae (e.g., ginger, turmeric), few had formal training in phytomorphology. Attitudes toward herbal medicine were generally positive, although confidence in counseling was limited by insufficient understanding of plant structure, taxonomy, and morphological markers related to pharmacological activity. Practices such as patient counseling and documentation remained inconsistent. The tables below remain unchanged from the original manuscript and present comparative data on global pharmacist KAP patterns (Tab. 2).
| Region | Average Knowledge Score (Self-reported or Objective) | Key Knowledge Gaps Identified |
| Europe | 55–70% correct answers | Limited in-depth pharmacology; herb–drug interactions |
| North America | 50–65% | Safety and efficacy of less commonly used herbs |
| Asia | 40–55% | Dosing, pharmacology, evidence-based guidelines |
| Middle East | 35–50% | Herb–drug interactions; lack of formal training |
| Africa | 25–40% | General pharmacological knowledge of herbs |
Table 2. Pharmacists’ knowledge scores across regions.
The search strategy yielded a total of 1,284 records, of which 67 full-text articles were assessed for eligibility, and 25 studies met the inclusion criteria for this review. These studies spanned multiple regions, including Europe (6), North America (4), Asia (7), the Middle East (5), and Africa (3). Sample sizes ranged from 100 to 600 participants, with the majority employing cross-sectional survey designs. While methodologies varied, the thematic synthesis revealed consistent patterns in pharmacists’ knowledge, attitudes, and practices toward herbal medicine, alongside clear regional differences.
Pharmacists’ knowledge of herbal medicine was generally low to moderate, with variations depending on geography and educational exposure. In Europe, pharmacists demonstrated relatively better knowledge, particularly regarding safety, dosing, and herb–drug interactions, although many still felt inadequately prepared to provide comprehensive counseling (Ng, et al. 2021). In Asia and the Middle East, studies revealed notable gaps in pharmacists’ ability to identify common herbal medicines or their adverse effects (Zaidi, et al. 2022, Letchumanan, et al. 2021). African studies highlighted particularly limited knowledge, often attributable to insufficient formal education and lack of reliable information sources (Oshikoya, et al. 2020).
Pharmacists’ attitudes were largely positive across most regions, with a strong recognition of the growing patient demand for herbal products. In the Middle East and Asia, pharmacists generally expressed supportive attitudes toward integrating herbal medicine into mainstream healthcare, though this was tempered by concerns over regulation and training. In Europe and North America, attitudes were more cautious, reflecting skepticism about the quality, efficacy, and safety of herbal remedies (Kwan, et al. 2006). African pharmacists often showed mixed attitudes, balancing cultural familiarity with herbal medicine against professional uncertainty (Tab. 3 and Tab. 4) .
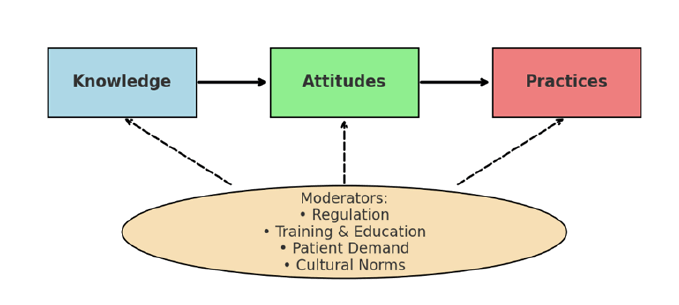
Despite positive or moderately supportive attitudes, pharmacists’ practices often fell short. Across most studies, pharmacists reported limited engagement in patient counseling regarding herbal medicine. In many cases, pharmacists dispensed herbal products passively, providing advice only when specifically asked by patients. Proactive counseling was rare, except in some European contexts where formal training and clearer regulatory frameworks were in place. In the Middle East and Asia, pharmacists often reported being uncomfortable counseling due to limited knowledge, while in Africa, counseling was minimal, with patients relying more on traditional practitioners (Fig. 1).
| Region | General Attitude | Key Influencing Factors |
| Europe | Cautious acceptance | Evidence base, liability concerns, patient safety |
| North America | Mixed; leaning skeptical | Safety concerns, regulatory gaps |
| Asia | Positive | Cultural acceptance, patient demand |
| Middle East | Positive | Religious and cultural norms, patient expectations |
| Africa | Mixed | Reliance on traditional healers, lack of confidence |
Table 3. Pharmacists’ attitudes toward herbal medicine.
| Region | Frequency of counseling | Main counseling behaviors | Reported barriers | Reported barriers |
| Europe | Moderate; 40-60% provide advice | Counseling on interactions, dosage, safety | Time constraints; insufficient training | Lack of training; poor regulations |
| North America | Low–moderate; 30–50% | Advice limited to safety concerns | Fear of liability; skepticism | Safety concerns; liability issues |
| Asia | Low; <30% provide regular advice | Dispensing only, little proactive counseling | Lack of training, poor guidelines | Lack of evidence-based guidelines |
| Middle East | Low–moderate; 25–40% | Basic information, often patient-initiated | Curriculum gaps, regulatory ambiguity | Concerns over efficacy and regulation |
| Africa | Very low; <20% | Rare counseling, minimal engagement | Limited training, cultural reliance on healers | Dominance of traditional healers; weak regulation |
Table 4. Pharmacists’ practices in herbal medicine counseling.
Figure 1. Conceptual framework of pharmacists’ knowledge, attitudes, and practices toward herbal medicine.
Description: This framework illustrates the dynamic relationship among Knowledge, Attitudes, and Practices (KAP). Pharmacists’ knowledge forms the foundation, influencing both their confidence and willingness to counsel patients. Positive attitudes may encourage practice, but insufficient knowledge often constrains its translation into professional behavior. Regulatory frameworks, educational exposure, and patient demand act as external moderators shaping these interactions.
Overall, this review shows that pharmacists worldwide recognize the importance of herbal medicine but lack consistent knowledge, which directly influences their ability to counsel patients. Attitudes are generally favorable, especially in culturally supportive regions, but practical engagement remains limited. Regional comparisons suggest that improvements in training, regulation, and evidence-based guidelines are crucial for empowering pharmacists to play a more active role in herbal medicine use.
Discussion
The global pattern observed in pharmacists’ KAP demonstrates persistent gaps in herbal medicine knowledge, particularly regarding plant identification and morphological characteristics. For pharmacists to accurately assess the safety and authenticity of herbal materials, a foundational understanding of plant morphology is essential. This includes recognizing leaves (example: German chamomile), stems (basil, mint), roots (ginger, turmeric, and licorice), flowers (chamomile, lavender, calendula, echinacea, and hibiscus), and microscopic features often used in pharmacognostic evaluations. Limited exposure to these concepts in pharmacy curricula contributes to pharmacists’ reduced confidence in advising patients, especially when evaluating unprocessed or minimally processed botanical materials. Incorporating phytomorphology training into pharmacy education and continuous professional development may enhance pharmacists’ engagement in herbal medicine counseling and improve public safety. Additionally, regulatory frameworks that mandate morphological authentication of herbal materials would further strengthen quality control across the herbal product supply chain.
The results demonstrate that pharmacists’ knowledge of herbal medicine is largely insufficient, particularly regarding herb–drug interactions, dosing, and adverse effects. This knowledge gap is most pronounced in the Middle East, Asia, and Africa, where pharmacy curricula often lack structured herbal pharmacology components. Similar findings in Europe and North America, though less severe, indicate that even in advanced pharmacy education systems, herbal medicine remains marginalized. These findings reinforce the need for formal integration of herbal medicine into undergraduate curricula and continuing professional development programs. Targeted training could strengthen pharmacists’ clinical competence and enable them to better meet patient needs.
Attitudes toward herbal medicine varied across regions, reflecting both cultural norms and the influence of scientific evidence. Pharmacists in Asia and the Middle East expressed supportive views, consistent with longstanding traditions of herbal use and patient expectations. By contrast, pharmacists in Europe and North America exhibited cautious or skeptical attitudes, reflecting concerns over efficacy, safety, and the absence of strong clinical guidelines. African pharmacists often expressed ambivalence, balancing respect for traditional healing practices with recognition of professional limitations. These findings highlight that while positive attitudes can drive engagement, skepticism can be equally valuable in ensuring patient safety particularly when it is grounded in evidence-based caution.
Despite moderate to positive attitudes, actual practice remains limited in most regions. Pharmacists commonly dispense herbal products passively and provide advice only when prompted by patients. Few studies reported proactive counseling or systematic documentation of herbal medicine use. This discrepancy between attitudes and practice is largely attributable to pharmacists’ lack of confidence, absence of clear clinical guidelines, and concerns over liability. The practice gap undermines the pharmacist’s role as a healthcare advisor and exposes patients to the risks of unsupervised herbal use.
The conceptual framework developed in this review emphasizes that pharmacists’ KAP is not shaped in isolation but is influenced by broader systemic factors. Regulation, training, patient demand, and cultural norms play crucial moderating roles. For example, in Europe, stricter regulations and professional liability concerns moderate pharmacists’ cautious engagement with herbal medicine. In the Middle East, strong patient demand and cultural norms encourage pharmacists to engage, but weak regulatory frameworks hinder safe practice. In Africa, the dominance of traditional healers limits pharmacists’ involvement, reflecting a unique cultural and systemic barrier (Posadzki, et al. 2013).
Taken together, the findings underscore the need for a more standardized global approach to herbal medicine in pharmacy practice. First, regulatory agencies should establish clear evidence-based guidelines to support pharmacists in providing safe counseling. Second, pharmacy education must address knowledge gaps by incorporating herbal medicine into core curricula and offering continuous education opportunities. Third, professional associations should promote clinical protocols that empower pharmacists to engage proactively with patients. By aligning education, regulation, and practice, pharmacists can be better equipped to manage herbal medicine within modern healthcare systems.
It is important to acknowledge limitations in the reviewed studies. Most relied on self-reported surveys, which may overestimate pharmacists’ knowledge and counseling practices. Furthermore, the heterogeneity of instruments used to measure KAP limited comparability across studies. Finally, regional gaps exist, particularly in Africa and Latin America, where few high- quality studies have been conducted. Future research should address these gaps through robust, standardized methodologies, including observational and intervention studies.
In summary, this review highlights a paradox: Pharmacists worldwide recognize the relevance of herbal medicine and often express supportive attitudes, yet their practices remain constrained by insufficient knowledge, weak regulatory support, and lack of training. Bridging this gap requires coordinated efforts at educational, regulatory, and professional levels. Empowering pharmacists through structured training and clear clinical guidelines will not only enhance their role in herbal medicine but also contribute to safer and more effective patient care.
Conclusion
This integrative review emphasizes that incorporating phytomorphology into pharmacy practice significantly enhances pharmacistsâ competence in handling herbal medicines. Understanding morphological traits of medicinal plants improves pharmacistsâ ability to assess authenticity, detect adulteration, and support evidence-based counseling. While global studies reveal positive attitudes toward herbal medicine, practical engagement remains limited due to insufficient training in plant structure and identification. Strengthening phytomorphological education, developing standardized guidelines, and improving regulatory oversight will empower pharmacists to play a more effective role in modern herbal medicine use.
The review reveals a global pattern: Pharmacists in regions with strong cultural traditions of herbal use, such as Asia and the Middle East, are more likely to hold positive attitudes but lack sufficient formal education to translate these into proactive practice. Conversely, pharmacists in Europe and North America demonstrate greater awareness of safety and interaction issues but remain cautious due to concerns about efficacy and liability. African pharmacists face unique challenges shaped by limited education and the dominance of traditional healers, resulting in minimal engagement.
Overall, the evidence underscores the urgent need for systemic reforms that strengthen pharmacists’ preparedness to manage herbal medicine. Educational curricula must integrate evidence-based herbal pharmacology, continuing professional development should provide ongoing updates, and regulatory bodies should establish clear guidelines for counseling and documentation. Such measures will not only empower pharmacists to assume a more proactive role but also ensure patient safety in an era of increasing herbal medicine use.
In conclusion, bridging the gap between pharmacists’ positive attitudes and their limited practices requires a coordinated global effort involving educators, policymakers, professional organizations, and pharmacists themselves. By enhancing knowledge, standardizing regulations, and fostering patient-centered counseling practices, pharmacists can fulfill their potential as frontline advisors in herbal medicine, thereby contributing to safer, more effective, and integrative healthcare systems.
References
- Maldonado Miranda JJ. (2021). Medicinal plants and their traditional uses in different locations. Phytomedicine. 207-223.
[Crossref]
- World Health Organization (WHO). (2019). WHO global report on traditional and complementary medicine 2019. WHO.
- Wachtel-Galor S, Benzie IFF. (2011). Herbal medicine: An introduction to its history, usage, regulation, current trends, and research needs.
[Google Scholar] [PubMed]
- Brantley SJ, Argikar AA, Lin YS, Nagar S, Paine MF. (2014). Herb-drug interactions: Challenges and opportunities for improved predictions. Drug Metab. 42:301–317.
[Crossref] [Google Scholar] [PubMed]
- Ng JY, Tahir U, Dhaliwal S. (2021). Barriers, knowledge, and training related to pharmacists' counselling on dietary and herbal supplements: A systematic review of qualitative studies. BMC Health Serv Res. 21:499.
[Crossref] [Google Scholar] [PubMed]
- Zaidi SF, Saeed SA, Khan MA, Khan A, Hazazi Y, Otayn M, Rabah M, Daniyal M. (2022). Public knowledge, attitudes, and practices towards herbal medicines; a cross-sectional study in Western Saudi Arabia. BMC Complement Med Ther. 22:326.
[Crossref] [Google Scholar] [PubMed]
- Khdour M, Kurdi M, Hallak H, Dweib M, Al-Shahed Q. (2018). Pharmacists' knowledge, attitudes, and practices towards herbal remedies in the West Bank: A cross-sectional study. The Lancet. 391:S17.
- Al-Jedai A, Qaisi S, Al-Meman A. (2016). Pharmacy practice and the health care system in Saudi Arabia. Can J Hosp Pharm. 69:231–237.
[Crossref] [Google Scholar] [PubMed]
- Kwan D, Hirschkorn K, Boon H. (2006). US and Canadian pharmacists’ attitudes, knowledge, and professional practice behaviors toward dietary supplements: A systematic review. BMC Complement Altern Med. 6:31.
[Crossref] [Google Scholar] [PubMed]
- Oshikoya KA, Oreagba IA, Awobusuyi JO, Popoola TD. (2020). Herbal medicine use and pharmacists’ role in sub-Saharan Africa: A narrative review. Trop J Pharm Res. 19: 1401–1410.
- Posadzki P, Watson L, Ernst E. (2013). Herb–drug interactions: An overview of systematic reviews. Br J Clin Pharmacol. 75:603–618.
[Crossref] [Google Scholar] [PubMed]