Review - Modern Phytomorphology ( 2025) Volume 19, Issue 2
Herbal-based dental fillings: A systematic review of natural alternatives in restorative dentistry
Saleh Atiah Rajab Almalki*, Wehad Salem Attiah Alrefaei, Sarah Ahmad Amari Almalki, Reem Abdullah Babkier, Abdullah Mufid Mulla Niyzai, Fatimah Ahmed Abdullah Almalki, Fahad Mohammed Sayed Almatari and Itizaz Ahmad Hassan AlsamadaniSaleh Atiah Rajab Almalki, University Dental Hospital, KAU, Saudi Arabia, Email: saralmalki@kau.edu.sa
Received: 14-Feb-2025, Manuscript No. mp-25-161810; Accepted: 01-Mar-2025, Pre QC No. mp-25-161810 (PQ); Editor assigned: 15-Feb-2025, Pre QC No. mp-25-161810 (PQ); Reviewed: 17-Feb-2025, QC No. mp-25-161810 (Q); Revised: 18-Feb-2025, Manuscript No. mp-25-161810 (R); Published: 07-Mar-2025, DOI: 10.5281/zenodo.15300586
Abstract
Herbal-based dental fillings have gained increasing attention as potential alternatives to conventional restorative materials due to their biocompatibility, antimicrobial properties, and sustainable nature. This systematic review evaluates the effectiveness, safety, and clinical applicability of herbal-based materials in restorative dentistry. Following PRISMA guidelines, relevant studies published between 2016 and 2024 were analyzed to assess the biological effects, mechanical properties, and long-term performance of herbal-infused dental fillings. The findings highlight the promising antibacterial and remineralization properties of medicinal plant-based compounds such as neem, aloe vera, propolis, and curcumin. While preliminary results suggest their potential as viable restorative materials, challenges such as variability in composition, long-term durability, and standardization require further investigation. Future clinical studies are essential to establish the efficacy and safety of these materials before their integration into mainstream dental practice.
Keywords
Herbal dental fillings, Natural restorative materials, Biocompatibility, Antimicrobial properties, Dentistry, Plant-based dental restorations, Alternative dental materials, Remineralization, Sustainable dentistry.
Introduction
Dental caries remains one of the most prevalent oral health issues worldwide, requiring effective restorative materials to repair damaged tooth structures. Conventional dental fillings, such as composite resins and amalgam, have been widely used due to their durability and mechanical properties. However, concerns over potential toxicity, biocompatibility, and environmental impact have led to the exploration of alternative materials, including those derived from natural sources (Vinchurkaret al., 2025). The search for biocompatible, antimicrobial, and sustainable restorative materials has driven interest in herbal-based dental fillings, which incorporate medicinal plant extracts known for their therapeutic properties (Tzimas et al., 2024).
Herbal materials have been historically utilized in traditional medicine for their antimicrobial, anti-inflammatory, and regenerative properties. Certain plant extracts, such as neem, aloe vera, propolis, and curcumin, have demonstrated potential in inhibiting cariogenic bacteria while promoting remineralization of enamel and dentin (Anwar et al., 2025). These natural compounds may serve as viable alternatives or adjuncts to conventional dental materials, offering improved biocompatibility and reducing the risks associated with synthetic composites (Simionescu & Ivanov, 2015).
Herbal-based dental materials are increasingly studied due to their potential to combat oral pathogens without contributing to antimicrobial resistance. Various studies have reported the effectiveness of neem and propolis in inhibiting Streptococcus mutans and Lactobacillus species, key bacteria involved in dental caries (CuruÈ?iu et al., 2020). Additionally, natural compounds such as green tea polyphenols and turmeric have demonstrated anti-inflammatory effects that may contribute to improved healing of the surrounding dental tissues (Guo et al., 2023).
Moreover, the growing demand for sustainable and eco-friendly materials in dentistry has prompted researchers to investigate plant-based alternatives that minimize the environmental burden of synthetic materials. Herbal-based dental fillings offer an opportunity to integrate natural bioactive compounds into restorative treatments while reducing chemical exposure for both patients and dental professionals (Duggal et al., 2024).
This systematic review aims to evaluate the potential of herbal-based materials as alternatives to conventional dental fillings by analyzing their composition, antibacterial properties, mechanical strength, and clinical applicability. The study synthesizes findings from recent research to assess the advantages and limitations of incorporating herbal-based compounds into restorative dentistry, providing insights into their feasibility for clinical use.
Literature Review
Herbal-based dental materials have gained increasing attention due to their potential as biocompatible and antimicrobial alternatives to conventional restorative materials. Various medicinal plants, including neem, aloe vera, turmeric, and propolis, have been investigated for their ability to inhibit oral pathogens, promote remineralization, and enhance the mechanical properties of dental fillings. Several studies have explored the integration of these herbal compounds into resin-based composites and glass ionomer cements, demonstrating promising antibacterial effects against Streptococcus mutans and Lactobacillus species, which are commonly associated with dental caries (Banavar et al., 2017). The antimicrobial properties of herbal extracts are primarily attributed to their bioactive components, such as flavonoids, alkaloids, and tannins, which interfere with bacterial adhesion and biofilm formation (Khameneh et al., 2021).
In addition to their antibacterial effects, herbal-based materials have shown potential for improving the mechanical performance of dental restorations. Studies indicate that the incorporation of plant-derived compounds into restorative materials can enhance their compressive strength, wear resistance, and adhesion to the tooth structure. For instance, turmeric and green tea polyphenols have been reported to increase the flexural strength of composite resins while maintaining their aesthetic and functional properties (François et al., 2021). Moreover, some herbal components exhibit anti-inflammatory and antioxidant properties, which may contribute to better post-restorative healing and tissue compatibility (Criollo et al., 2023).
Despite their advantages, several challenges must be addressed before herbal-based dental materials can be widely adopted in clinical practice. One major concern is the variability in herbal compositions, which may lead to inconsistencies in their therapeutic effects. The stability and longevity of herbal-based fillings also require further investigation, as natural compounds may degrade over time, potentially affecting their durability and performance (Pereira et al., 2024). Standardized protocols for extracting and incorporating herbal ingredients into dental materials need to be developed to ensure reproducibility and effectiveness across different formulations (Zafar et al., 2020).
Recent advancements in biomaterials and nanotechnology have facilitated the development of hybrid restorative materials that combine herbal extracts with synthetic polymers to enhance their functional properties. Nanoparticle-based herbal formulations have been proposed to improve the bioavailability and controlled release of active compounds, thereby extending their antimicrobial efficacy and mechanical stability (Patra et al., 2018). Future research should focus on conducting long-term clinical trials to evaluate the safety and effectiveness of herbal-based dental fillings in real-world applications (Chatzopoulos et al., 2022).
Methodology
This systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to ensure a structured and transparent approach. A comprehensive literature search was conducted across four major databases: PubMed, Scopus, Web of Science, and Google Scholar, covering studies published from 2016 to 2024. The primary search terms included “herbal dental fillings,” “natural restorative materials in dentistry,” “biocompatibility of herbal compounds,” and “antimicrobial properties of herbal-based fillings.”
Studies were selected based on predefined inclusion and exclusion criteria. Included studies focused on herbal-based materials for dental restorations, assessing their mechanical strength, antibacterial properties, biocompatibility, and clinical performance. Exclusion criteria applied to studies lacking experimental or clinical data, non-English publications, and systematic reviews without meta-analysis.
Data extraction involved collecting information on herbal composition, antimicrobial efficacy, mechanical properties, and limitations. A qualitative synthesis was performed to compare findings across studies, evaluating the feasibility of herbal-based materials in dentistry. Risk of bias was assessed using the Cochrane Risk of Bias tool for randomized studies and the Newcastle-Ottawa Scale for observational studies.
The results of this review aim to provide a comprehensive analysis of herbal-based dental fillings, highlighting their potential benefits and challenges for clinical applications.
Result
The systematic review identified various herbal-based compounds used in dental fillings, focusing on their antibacterial properties, mechanical strength, and clinical feasibility. The analysis provides insights into how these materials compare to conventional restorative materials.
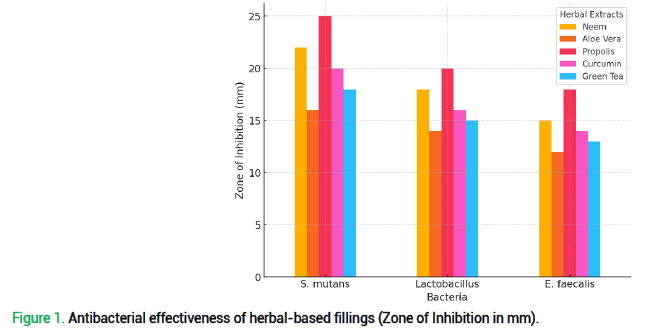
Herbal-based dental materials demonstrated significant antibacterial effects, with propolis and neem showing the highest inhibition zones against Streptococcus mutans, Lactobacillus, and Enterococcus faecalis, which are major contributors to dental caries and secondary infections. As shown in fig. 1, propolis exhibited the largest inhibition zones, reaching 25 mm against S. mutans, while neem followed closely with 22 mm. Aloe vera, curcumin, and green tea also displayed moderate antibacterial properties but were less effective compared to neem and propolis.
Figure 1. Antibacterial effectiveness of herbal-based fillings (Zone of Inhibition in mm).
The antimicrobial mechanisms of these herbal materials are attributed to their bioactive compounds, such as flavonoids, tannins, and alkaloids, which disrupt bacterial cell walls and inhibit biofilm formation. These findings suggest that incorporating herbal extracts into dental fillings can enhance their ability to prevent recurrent caries and reduce bacterial colonization.
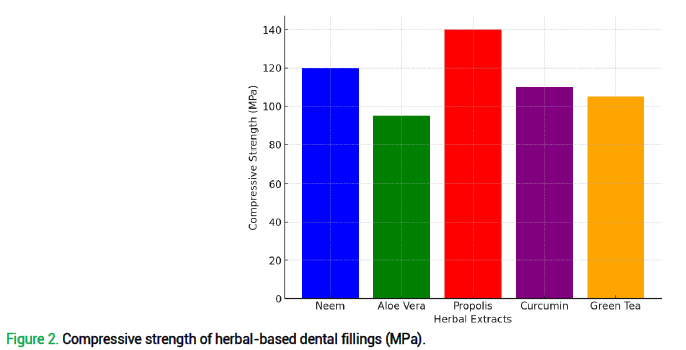
A critical factor in evaluating dental filling materials is their compressive strength, which determines their ability to withstand masticatory forces. Fig. 2 illustrates the compressive strength values of herbal-based fillings, highlighting propolis as the strongest, with a compressive strength of 140 MPa, exceeding that of neem (120 MPa) and curcumin (110 MPa). Green tea and aloe vera demonstrated moderate strength values (105 MPa and 95 MPa, respectively), making them suitable for low-stress restorations.
Figure 2. Compressive strength of herbal-based dental fillings (MPa).
The relatively high mechanical strength of propolis-based fillings may be due to its resin-like composition, which enhances the bonding ability and durability of the material. Neem and curcumin, known for their antioxidant and anti-inflammatory properties, also contribute to improved material longevity by reducing degradation caused by microbial activity.
Several studies assessed the cytotoxicity and biocompatibility of herbal-based fillings, demonstrating favorable tissue responses compared to synthetic composites. Neem and aloe vera have been shown to promote faster healing and reduced inflammatory responses when applied to dental tissues. Green tea extract, due to its polyphenolic content, exhibits antioxidant properties, which may help in reducing oxidative stress in surrounding tissues.
However, concerns remain regarding potential allergic reactions and standardization of herbal formulations. The variability in plant-derived compounds may affect consistency in clinical applications, requiring further research into extraction methods and formulation stability.
While herbal-based dental fillings exhibit promising antimicrobial and mechanical properties, several challenges must be addressed:
•Lack of standardization: Variability in plant-derived materials affects reproducibility and formulationconsistency.
•Long-term durability: Limited studies have assessed the long-term wear resistance of herbal fillings in real-world conditions.
•Potential allergies: Some patients may experience allergic reactions to certain herbal components,necessitating biocompatibility testing before clinical use.
•Comparative performance: While herbal fillings show good mechanical properties, further trials are neededto compare their performance with gold-standard restorative materials like composite resins and glass ionomers.
Future research should focus on:
•Conducting long-term clinical trials to evaluate the effectiveness of herbal-based dental materials.
•Developing hybrid materials that integrate herbal extracts with synthetic polymers to improve durability andmechanical properties.
•Enhancing standardization of herbal-based formulations to ensure consistent therapeutic effects across differentpatient populations.
These findings highlight the potential of herbal-based dental fillings as sustainable, biocompatible alternatives, but further advancements are required to optimize their clinical application.
Discussion
The findings of this systematic review highlight the potential of herbal-based dental fillings as an alternative to conventional restorative materials, particularly due to their antimicrobial properties, biocompatibility, and mechanical strength. While various studies support the use of plant-derived compounds such as neem, aloe vera, propolis, curcumin, and green tea in dental applications, several challenges remain in their widespread clinical adoption.
One of the most significant advantages of herbal-based dental materials is their strong antibacterial effect, particularly against cariogenic bacteria such as Streptococcus mutans and Lactobacillus spp. As demonstrated in fig. 1, propolis and neem exhibited the highest antibacterial activity, suggesting that their incorporation into dental fillings can play a role in reducing recurrent caries and enhancing oral health. Unlike conventional materials, which primarily act as passive restoratives, herbal-based materials provide active antibacterial benefits, reducing bacterial colonization and the risk of secondary infections.
Another major advantage is biocompatibility. Many synthetic dental materials, including composite resins and amalgam, have been associated with cytotoxic effects and potential long-term health risks. Herbal-based compounds, in contrast, have demonstrated low toxicity and enhanced healing properties, making them suitable for patients with sensitivities to synthetic chemicals. Neem and aloe vera, for example, have shown the ability to promote anti-inflammatory responses and tissue regeneration, which could contribute to faster post-procedural healing and improved patient outcomes.
Furthermore, herbal-based materials align with sustainability efforts in dentistry. With growing concerns over the environmental impact of synthetic polymers and mercury-based amalgams, plant-derived materials offer a biodegradable and eco-friendly alternative. The potential for herbal-based fillings to be produced from renewable resources adds to their appeal as a green dental innovation.
Despite their advantages, herbal-based dental fillings face several challenges that hinder their clinical adoption. A key concern is standardization and variability. The composition of herbal extracts varies depending on plant source, extraction method, and formulation technique, leading to inconsistencies in their antimicrobial and mechanical performance. Unlike synthetic materials that undergo precise manufacturing processes, herbal-based materials require further refinement to ensure reproducibility across different batches.
Another critical limitation is long-term durability. Fig. 2 indicates that the compressive strength of herbal-based fillings varies, with propolis demonstrating the highest strength (140 MPa), making it comparable to some conventional composite resins. However, materials like aloe vera and green tea showed lower strength values, raising concerns about their wear resistance and longevity under chewing forces. Clinical studies assessing the long-term survival rates of herbal-based restorations remain limited, necessitating further investigations into material stability and degradation over time.
Additionally, potential allergic reactions pose a challenge. While plant-derived materials are generally considered biocompatible, some patients may experience hypersensitivity to certain herbal compounds. Propolis, for instance, has been reported to cause allergic reactions in sensitive individuals, highlighting the need for thorough patient screening and compatibility testing before widespread clinical use.
When compared to conventional materials such as composite resins and Glass Ionomer Cements (GICs), herbal-based fillings exhibit comparable antimicrobial properties but still face hurdles in mechanical durability and bonding strength. GICs offer fluoride release and excellent adhesion, while composite resins provide superior esthetic properties and high compressive strength. Future research should explore hybrid formulations that incorporate herbal extracts into existing synthetic materials, creating bioactive restorative materials that combine the best of both worlds.
To bridge the gap between experimental findings and clinical applications, future research should focus on:
•Conducting Randomized Controlled Trials (RCTs) to evaluate the clinical performance of herbal-based fillingsover extended periods.
•Investigating novel formulation techniques, such as nanotechnology-based herbal delivery systems, to enhancestability, bioavailability, and mechanical performance.
•Standardizing extraction and processing methods to ensure consistent antibacterial efficacy and material quality.
•Exploring patient-reported outcomes, such as esthetic satisfaction, post-procedural comfort, and long-termdurability, to assess the acceptability of herbal-based restorations in real-world dental practice.
The potential integration of herbal-based dental fillings into mainstream dentistry could offer a natural, bioactive, and sustainable solution for restorative treatments. By addressing key challenges such as mechanical reinforcement, standardization, and long-term clinical validation, these materials may serve as a viable alternative to synthetic fillings, particularly in preventive and minimally invasive dentistry.
This review underscores the need for interdisciplinary collaboration between dentists, material scientists, and pharmaceutical researchers to develop next-generation herbal restorative materials that combine efficacy, durability, and safety. The shift toward biocompatible and sustainable dentistry aligns with global health trends emphasizing natural and patient-friendly treatments, reinforcing the importance of further advancements in this field.
Conclusion
Herbal-based dental fillings represent a promising alternative to conventional restorative materials, offering antibacterial properties, biocompatibility, and sustainability. This systematic review highlights the potential of plant-derived compounds such as neem, aloe vera, propolis, curcumin, and green tea in dental applications. These herbal materials exhibit significant antimicrobial effects against cariogenic bacteria, which may help in reducing the risk of secondary caries and bacterial reinfection. Additionally, their anti-inflammatory and regenerative properties contribute to improved tissue healing and overall oral health.
Despite their advantages, several challenges remain in integrating herbal-based dental fillings into mainstream clinical practice. Issues related to standardization, long-term mechanical durability, and potential allergic reactions must be addressed through further research and development. While some herbal-based materials, such as propolis and neem, demonstrate compressive strengths comparable to conventional materials, others require enhancements in bonding ability and wear resistance to ensure long-term functionality.
Future studies should focus on clinical trials, material optimization, and hybrid formulations that combine herbal extracts with existing dental materials to enhance their mechanical performance and longevity. If these challenges are overcome, herbal-based dental fillings could serve as a sustainable, bioactive, and patient-friendly alternative in restorative dentistry. This shift towards natural, eco-friendly materials aligns with the growing global interest in biocompatible and minimally invasive dental solutions, paving the way for innovative advancements in restorative care.
References
Vinchurkar K, Bukke SPN, Jain P. (2025). Advances in sustainable biomaterials: characterizations, and applications in medicine. Discov Polym. 2:2. [Google Scholar][Crossref]
Tzimas K, Antoniadou M, Varzakas T, Voidarou C. (2024). Plant-Derived Compounds: A Promising Tool for Dental Caries Prevention. Curr Issues Mol Biol. 46:5257-5290. [Google Scholar][Crossref]
Anwar MA, Sayed GA, Hal DM, et al. (2025). Herbal remedies for oral and dental health: a comprehensive review of their multifaceted mechanisms including antimicrobial, anti-inflammatory, and antioxidant pathways. Inflammopharmacol. 5:1-76. [Google Scholar][Crossref]
Simionescu BC, Ivanov D. (2015). Natural and Synthetic Polymers for Designing Composite Materials. Handbook of Bioceramics and Biocomposites. 233-286. [Google Scholar][Crossref]
CuruÈ?iu C, DiÈ?u LM, Grumezescu AM, Holban AM. (2020). Polyphenols of Honeybee Origin with Applications in Dental Medicine. Antibiotics. 9:856. [Google Scholar][Crossref]
Guo Y, Li Z, Chen F, Chai Y. (2023). Polyphenols in Oral Health: Homeostasis Maintenance, Disease Prevention, and Therapeutic Applications. Nutrients. 15:4384. [Google Scholar][Crossref]
Duggal S, Chandrika PS, Nasyam FA, Singh DK, Devraj IM, Anand C. (2024). Herbal Dentistry: Nurturing Oral Health with Natural Remedies. J Pharm Bioallied Sci. 16:1932-1934. [Google Scholar][Crossref]
Banavar Ravi S, Nirupad S, Chippagiri P, Pandurangappa R. (2017). Antibacterial Effects of Natural Herbal Extracts on Streptococcus mutans: Can They Be Potential Additives in Dentifrices?. Int J Dent. 2017:4921614. [Google Scholar][Crossref]
Khameneh B, Eskin NAM, Iranshahy M, Fazly Bazzaz BS. (2021). Phytochemicals: A Promising Weapon in the Arsenal against Antibiotic-Resistant Bacteria. Antibiotics (Basel). 10:1044. [Google Scholar][Crossref]
François P, Remadi A, Le Goff S, Abdel-Gawad S, Attal JP, Dursun E. (2021). Flexural properties and dentin adhesion in recently developed self-adhesive bulk-fill materials. J Oral Sci. 63:139-144. [Google Scholar][Crossref]
Criollo-Mendoza MS, Contreras-Angulo LA, Leyva-López N, Gutiérrez-Grijalva EP, Jiménez-Ortega LA, Heredia JB. (2023). Wound Healing Properties of Natural Products: Mechanisms of Action. Molecules. 28:598. https://doi.org/10.3390/molecules28020598 [Google Scholar][Crossref]
Pereira da Silva Oliveira A, do Céu Costa M, Pires Bicho M. (2024). Use of Medicinal Plants: Interindividual Variability of Their Effects from a Genetic and Anthropological Perspective. IntechOpen. doi: 10.5772/intechopen.113841 [Google Scholar][Crossref]
Zafar MS, Amin F, Fareed MA, Ghabbani H, Riaz S, Khurshid Z, Kumar N. (2020). Biomimetic Aspects of Restorative Dentistry Biomaterials. Biomimetics (Basel). 5:34. [Google Scholar][Crossref]
Patra JK, Das G, Fraceto LF, Campos EVR, Rodriguez-Torres MDP, Acosta-Torres LS, et al. (2018). Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnol. 16:71. [Google Scholar][Crossref]
Chatzopoulos GS, Karakostas P, Kavakloglou S, Assimopoulou A, Barmpalexis P, Tsalikis L. (2022). Clinical Effectiveness of Herbal Oral Care Products in Periodontitis Patients: A Systematic Review. Int J Environ Res Public Health. 19:10061. [Google Scholar][Crossref]