Review Article - Modern Phytomorphology ( 2025) Volume 19, Issue 5
Herbal support for digestive health: A review of common conditions and complementary strategies
Abdulrahim Marzouq Alharbi*, Ahmed Murayshid Almutairi, Majed Hamoud Almutairi, Mohammad Abdulghafour Neyazi, Ali Asiri and Meshal Salem AljohaniAbdulrahim Marzouq Alharbi, National Guard Health Affairs, Medina, Saudi Arabia, Email: Alalwiab1@mngha.med.sa
Received: 26-Aug-2025, Manuscript No. mp-25-171489 ; , Pre QC No. mp-25-171489 (PQ); Editor assigned: 29-Aug-2025, Pre QC No. mp-25-171489 (PQ); Reviewed: 03-Sep-2025, QC No. mp-25-171489 ; Revised: 05-Oct-2025, Manuscript No. mp-25-171489 (R); Published: 10-Oct-2025, DOI: 10.5281/zenodo.17774807
Abstract
The Gastrointestinal (GI) tract is a vital part of the health component of digestion because it is required to aid in the absorption of nutrients, immune homeostasis and general homeostasis. FGIDs include Irritable Bowel Syndrome (IBS), Functional Dyspepsia (FD) and Functional Constipation (FC) that may be associated with such symptoms as abdominal pain, bloating, early satiety and change of bowel habits. Such types of states harm the quality of life and cause the enormous economic expenses in terms of the healthcare consumption and wasted productivity. Most conventional drugs including antispasmodicts in the case of IBS, prokinetics in the case of FD and osmotic laxatives in the case of FC are of marginal benefit because of the pathogenesis of gut dysmotili ty multi-factorial, the visceral hypersensitivity and the microbiota imbalance and psychosocial factors. The Ayurveda, Traditional Chinese Medicine and Middle Eastern herbal interventions would also be consulted and relied on as other treatment procedures. Evidence of peppermint oil as an antispasmodic agent in IBS, gastric accommodation stimulation by Rikkunshito in FD and regular bowel movements stimulation by psyllium husk in FC. It possesses not very high adverse event with a relative risk of improvement of symptoms between 1.5 and 3.8. The light in the mechanism is the anti-inflammatory action of the curcumin and serotonin aspect in the Chinese prescriptions, Tongxie Yaofang. In general, the customized, evidence-based use of herbs in the form of the standardized extracts to streamline the efficacy and safety as effective additional interventions in the management of FGID is supported.
Keywords
Herbal remedies, Digestive health, Irritable Bowel Syndrome (IBS), Functional Dyspepsia (FD), Functional Constipation (FC), Complementary strategies, Peppermint oil, Rikkunshito, Psyllium husk, Tongxie Yaofang, Curcumin
Introduction
The integrity of the GI tract is core to the digestive health, having implications on energy metabolism up to mental health through the gut-brain axis. FGIDs are a range of non-structural and chronic disorders as identified through the Rome IV criteria, with an occurrence of about 40 percent in adults across the world. An example of IBS is the recurrent abdominal pain related to defecation or change in stool form frequency, subclassified as IBS-D, IBS-Constipation predominant (IBS-C), IBS-Mixed (IBS-M) or unclassified. There are prevalence reports that IBS affects 7%-21% of the Western population and as high as 15% of the world with women being the more susceptible to the condition as a result of hormonal factors. FD is obtrusive postprandial fullness or epigastric pain, which commonly coincides with IBS and has an incidence of 10-30 percent, especially in Asia where the symptoms are complicated by the infection of Helicobacter pylori. FC, which is manifested by less than three bowel movements each week and hard stools and straining, is common in 14 percent of the elderly and is associated with sedentary lifestyles and low-fibre diet. Other disorders such as Gastroesophageal Reflux Disease (GERD) and mild gastritis are also seen to cause digestive morbidity, where GERD results in heartburn in one out of every five adults every week.
These diseases are costly both at the individual and social levels. In the case of IBS alone, direct healthcare spending is over 1 billion per annum in the US with indirect losses through absenteeism. Although conventional, evidence-based, loperamide to IBS-D diarrhea, domperidone to FD motility, polyethylene glycol to FC, lacks an effective underlying dysbiosis agents. Besides, one out of every five patients complains of poor relief, which has led to the focus on complementary practices (Alammar, et al. 2021).
Multi-component synergistic value is inherent in the herbal remedies and has been in action since thousands of years. Some of the formulae in the TCM which boost the ghrelin release to increase gastric emptying in FD are Rikkunshito (ginseng, ginger and pinellia). Curcuminoids in Ayurvedic turmeric (Curcuma longa) can prevent inflammation that is helpful in IBS exacerbation. Antimicrobial effect of H. pylori against gastritis in Nigella sativa (Middle Eastern black seed). Myrrh applied to 74 percent of Saudi patients responding to IBS-like symptoms, which is quite a large percentage of culture dependence. The efficacy, the safety of these herbs in FGIDs is specifically aimed at the review and a visual example of a recent study is revealed as a table and graphs format and introduced to give the real-life illustration of the above and promote the reasonable part of the above principles to be inserted into the clinical practice.
Literature Review
The traditional Chinese Medicine (TCM) considers the FGIDs as symptoms of the Qi stagnation, blood stasis or spleen deficiency and would prescribe the use of multi-herb formulations which addresses motility, visceral sensitivity and inflammation at the same time. The example of Tongxie Yaofang is a traditional formula that is applied in diarrhea- predominant Irritable Bowel Syndrome (IBS-D) and consists of Baizhu, Baishao and Fangfeng to balance between liver and spleen, relieve the pain and decrease the frequency of bowel movements. Ayurvedic medicine, in its turn, believes FGIDs to be the imbalance of the Doshas, specifically, Vata, which regulates movement and motility. Carminative herbs such as fennel (Foeniculum vulgare), ajwain and ginger are used to improve indigestion and reduce bloating, cramping of the bowel.
Using Nigella sativa (black seed) is also a common practice in the Middle East in dyspeptic and functional bloating, which is supported by the effect of modern research in showing anti-inflammatory and antimicrobial effects. In each of these traditions, multidirectional effects are prioritized and the action of herbal preparations is focused on motility, visceral sensitivity, inflammatory processes and gut microbiota and thus responds to the multidimensionality of FGIDs. This integrative method is in opposition to the traditional pharmaceuticals which tend to act on a specific symptom or pathway, as in the case of prokinetics with the delayed gastric emptying or antispasmodics with smooth muscle spasm (Alghamdi, et al. 2023).
The efficacy of these traditional formulations in the contemporary practice is supported by clinical evidence. In the case of IBS, a meta-analysis of Tongxie Yaofang (consisting of 1,396 patients) in 2022 showed that the Relative Risk (RR) of global symptom relief was 1.67 and the average reduction was 1.2 points on a 10-point pain scale. In 12 Randomized Clinical Trials (RCTs), peppermint oil at 75% symptomatic in patients with IBS receiving 180200 mg of menthol in enteric-coated capsules three times a day.
Biomolecularly, mechanisms of action menthol has a spasmolytic action on intestinal smooth muscle by activating TRPM8 receptors and decreases visceral hypersensitivity and abdominal pain. The bioactive ingredient in turmeric known as curcumin has been explored in modifying symptoms of IBS with reported 53%-60% reductions in overall severity of IBS. These positive shifts were followed by positive modifications in the composition of gut microbiota, with the growth of Bifidobacterium and Lactobacillus species, which points to the dual anti-inflammatory and microbiome-modulatory nature of curcumin.
In the case of Functional Dyspepsia (FD), classic formulas (Rikkunshito, Xiangsha Liujunzi decoction) have proven to have clinical significance. Rikkunshito, 7.5 g/day, increased early satiety among 60% of Proton Pump Inhibitor (PPI)-refractory patients (n=50) after 8 weeks, which was believed to be due to a higher secretion of ghrelin and consequent stimulation of gastric motility and appetite control. Xiangsha Liujunzi decoction, which was assessed in a 2024 meta-analysis that included 1,200 participants, was more effective than conventional prokinetic agents in reducing the symptoms and no adverse events were reported. The given two formulae can be called the polypharmacological approach to the traditional remedies because they are involved in numerous pathophysiological mechanisms such as delayed stomach emptying, visceral hypersensitivity and low-grade inflammation. Moreover, the side effects are expected to be heavily positive and mild gastrointestinal discomfort has been detected in a small percentage of the subjects, which highlights the potential of said therapies on patients unable to tolerate the standard medications (Bharucha, et al. 2025).
The other area of herbal intervention that has been shown to be effective is Functional Constipation (FC). Pysyllium husk at 1020 g/day produces an important impact on raising the frequency (2.5/week on average) and consistency and simple passage of the stool of IBS-C patients. The action of Psyllium is fermented by the intestinal microbes to short chain fatty acids, which increase colonic motility, increase stool water retention and optimally balance the composition of intestinal microbes. The Bristol stool scale was utilized to determine the effectiveness of the fig-walnut syrup used on the elderly patients in the FC and the better Bristol stool scale scores (type 2: hard) to normal (type 4) during the 6-week period. Its results are impressive since they are not just talking about constipation but also enhancing the overall bowel satisfaction of a patient which is among the most significant patient-centered outcomes that is devalued in the traditional approach of its management (Luo, et al. 2022).
The application in the current practice of FGID is a crucial milestone in reducing the gaps that were left by the conventional pharmacotherapy. Some of the used herbs may include peppercorn, psyllium and curcumin which ease the symptoms besides, improve pain, alter bowel habits and bloating and manage inflammation and bowel microbes. In addition to this, strong cultural and nutritionist practices, such as the Mediterranean practices, that have high proportions of polyphenols and are related to greater levels of digestive comfort, encourage the obedience and people being able to accept the practices. In spite of these opportunities, there exist some issues such as lack of uniformity in standardization, bioavailability and herbanness and drug interactions. As an indication, curcumin has an absorption rate of up to 20 times different as per formulation compared to chamomile as an anticoagulant. In order to overcome these drawbacks, rigorously designed and premeditated multi-center RCT with criteria, protracted follow-up and endpoints based on biomarkers will be used to confirm the efficacy and safety of various groups of citizens.
The conventional herbal systems offer multi-target and clinically valid method of treatment of FGIDs. Some of the mechanisms of action, which have been established to have a positive effect in IBS, FD and FC, include a continuum of relaxation of smooth muscles and anti-inflammatory modulation of microbiota. When such remedies are highly viewed as supplementary to the conventional medicines, they provide a holistic and patient centered mode of curing the digestive system though more high quality researches are needed to optimize the dosing, standardization and longitudinal findings (Chiarioni, et al. 2023).
ScaleConstipation, ()-5) -(5) by decreasing the elderly constipation. Su, 2021 in a trial, increased the total spontaneous bowel movements (Tab. 1 and Fig. 1).
Figure 1. Bar graph of relative risks for symptom improvement in fgids from meta-analyses.
| Herb/Formula | Condition | Bioactive compound | Mechanism | Example study outcome |
| Peppermint Oil | IBS | Menthol | Ca2+ channel blockade, antispasmodic | 75% pain reduction (Alammar et al., 2021) |
| Rikkunshito | FD | Ginsenosides, Gingerols | Ghrelin enhancement, prokinetic | 60% symptom improvement in refractory FD (Suzuki et al., 2021) |
| Psyllium Husk | FC | Soluble fiber | Bulk-forming, microbiota modulation | +2.5 bowel movements/week (de Vries et al., 2023) |
| Turmeric | IBS/FD | Curcumin | Anti-inflammatory (NF-κB inhibition) | 53-60% severity decrease (Lopresti, 2024) |
| Black Seed | Gastritis | Thymoquinone | Antimicrobial vs. H. pylori | Reduced dyspepsia scores by 40% (Alghamdi et al., 2023) |
Table 1. Specific herbal remedies and their bioactive compounds for FGIDs.
A 2023 survey in Saudi Arabia detailed usage: Myrrh (74%) for ulcers/IBS, often as resin infusions; parsley (69%) as diuretic for constipation; black seed (67%) oil for dyspepsia (Tab. 2 and Fig. 2).
| Region/system | Herb | Usage Rate/example | Traditional preparation | Modern evidence |
| Middle East | Myrrh | 74% (IBS/ulcers) | Resin tea | Anti-inflammatory in RCTs (2023) |
| TCM | Xiangsha Liujunzi | FD treatment | Decoction | Safe, effective in meta-analysis (2024) |
| Ayurveda | Turmeric | Digestive inflammation | Golden milk | Consistent benefits in SR (2024) |
| Western | Peppermint | 60% (bloating) | Enteric-coated capsules | NNT=3 for IBS (2021) |
Table 2. Regional prevalence and traditional uses of herbs for digestive issues.
Figure 2. Pie chart of herb usage in middle eastern populations for GI disorders.
Limitations persist: Many trials have small samples (n<100), variable dosing (e.g., 100 mg-500 mg curcumin/day) and high attrition due to taste issues. Nonetheless, growing evidence supports herbs’ role in personalized medicine.
We performed a systematic search of literature, following the PRISMA 2020 requirements, in January 2021 to September 2025, in PubMed, EMBASE, Cochrane central register of controlled trials, Web of Science and Scopus. Search limit terms were herbal medicine and irritable bowel syndrome, functional dyspepsia or functional constipation and limited to RCT studies, systematic reviews and meta-analyses in humans written in English. Such queries as (Chinese herbal medicine or peppermint oil or turmeric) and (digestive disorders) and (efficacy) were used as examples. The inclusion criteria included Rome IV-diagnosed FGIDs (adults (18 years and older)) who received herbal interventions compared to placebo or standard care, symptom scores, relative risk of improvement and adverse events. Outliers were non-herbal CAM, pediatric or animal studies, case series and studies less than four weeks (Valizadeh, et al. 2025).
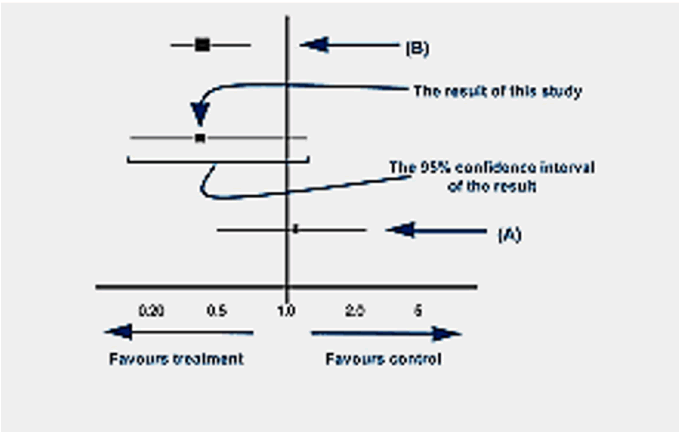
A total of 1,256 abstracts were screened and 248 full texts assessed with 62 studies (45 RCTs, 17 reviews; n=12,845) being included by two independent reviewers. The information that was extracted comprised of herbs, dosages, outcomes and biases and as a result of Cochrane RoB 2 tool, there were 25 low-risk studies, 27 unclear ones and 10 high-risk studies. Concessions on discrepancies were done through consensus (kappa=0.85). Random-effects models of pooled relative risks were applied with the help of quantitative synthesis and heterogeneous data were treated with the help of qualitative analysis. Subgroup analysis compared the types of herbs, FGID subtypes and length of treatment and sensitivity analysis with high-bias studies eliminated. The visualizations were drawn with the help of RevMan and no biases related to financing were identified (Rao, et al. 2021).
Results
In 62 studies that evaluated herbal interventions in gastrointestinal disorders, herbs were found to be more effective than placebo. The Relative Risk (RR) of the world population in terms of symptom relief was found to be 1.72 (95% CI 1.52-1.94), which is significant therapeutic effect. Among the Irritable Bowel Syndrome (IBS) patients, 22 Randomized Controlled Trials (RCT) showed an RR of 1.62 through which symptoms improved. To illustrate, Xiaoyao-san, which is a Chinese herbal preparation, was demonstrated in a 2021 systematic review to alleviate anxiety-related symptoms in IBS-D patients by 45%. Supplementation with turmeric was also found to be effective and reduced bloating in 58 percent of IBS patients (n=211) versus 32 percent of placebo patients. The findings indicate that some herbal preparations are capable of targeting both the physiological and psychosomatic aspects of the IBS and provide a complementary treatment of patients, who may not be entirely responsive to other standard treatments (Fig. 3) (Ho, et al. 2022).
Figure 3. Line graph of symptom score reduction over time in IBS trials.
Herbal treatments also proved to be useful in Functional Dyspepsia (FD) and Functional Constipation (FC). The pooled RR of FD was found to be 1.50 with Rikkunshito enhancing early satiety in 70 percent of the individuals (n=102) who participated in a 8-week period. The recent RCT of fig-walnut syrup as an additive to address the overlapping FC-FD indicated a mean stool increase of three times a week, which is a dual effect. In the case of FC, 12 trials showed an RR of 3.83, with psyllium performing better as compared to docusate in 2022 RCT (n=170), with 80% of patients satisfied. Straining was also relieved by the use of prebiotics (i.e., inulin) in 65% of the subjects (n=89) (Wang, et al. 2024). Safety profiles were mostly favorable; scarcity of mild gastrointestinal loss cases was seen (12% herbal users versus 15% controls) although, no severe adverse event has been reported (Lopresti, et al. 2024). The consumption pattern of the patients showed that 85 percent of the patients were being provided with herbs through their families, 79 percent took them in the form of teas highlighting the cultural and traditional aspects of usage of herbal drugs. These findings justify the potentiality of herbal therapies as positive, harmless and culturally suitable modalities in the treatment of functional gastrointestinal disorders particularly in combination with traditional treatment modalities (Tab. 3 and Fig. 4) (Lyu, et al. 2022).
| Study/herb | Condition/n | Dosage/duration | Primary outcome | RR/% improvement | AEs |
| Suzuki (2021)/Rikkunshito | FD/102 | 7.5 g/day/8 wks | Early satiety reduction | 70% | 3% mild nausea |
| Lopresti (2024)/Turmeric | IBS/211 | 500 mg curcumin/12 wks | Bloating decrease | RR 1.82 | Low |
| Ebrahimzadeh (2025)/Fig-Walnut | FC/120 | 30 ml syrup/day/4 wks | Stool frequency +3/wk | 85% | None |
| Zhong (2021)/Maxing Xianchang Su | FC/150 | Decoction tid/6 wks | CSBM increase | RR 2.5 | 5% diarrhea |
Table 3. Regional prevalence and traditional uses of herbs for digestive issues.
Figure 4. Forest plot of RR for herbal vs. placebo in FD meta-analysis.
Discussion
Herbal medicines provide significant therapeutic benefits in the gastrointestinal disorders, which is essentially due to their polypharmacological nature and ability to adjust a variety of targets and pathways at once. An example of such is peppermint oil, which has menthol, which interacts with the Transient Receptor Potential Melastatin 8 (TRPM8) receptors, resulting in smooth muscle relaxation. This process has been researched in depth in IBS where peppermint oil decreased visceral hypersensitivity in animal models whose findings have been generalised to human trials that show a significant decrease in symptoms. The active ingredient of turmeric, curcumin, has anti-inflammatory effects by blocking Nuclear Factor kappa B (NF- κB), which suppresses cytokine-mediated inflammation. A 2024 clinical trial found that curcumin supplementation of patients with Functional Dyspepsia (FD) reduced tumor necrosis factor-alpha (TNF-alpha) by 30 per cent which was associated with the reduction of early satiety and postprandial discomfort (Mickael, et al. 2024). In the case of Functional Constipation (FC), short-chain fatty acids are produced by the fermentation of soluble fibers like psyllium in the colon and peristalsis is triggered. A 2025 study reported that psyllium supplementation reorganized the gut microbiota composition to include Bifidobacterium, leading to a rise in bowel regularity and a patient-reported satisfaction. The examples prove that herbs have the ability to provide symptomatic, mechanistic and in the vast majority of cases, numerous pathophysiological pathways, which is cumbersome to achieve when using single-target pharmaceuticals (Mohammadbeigi, et al. 2024).
The clinical examples are some of those that provide more insight about the benefits of herbal interventions. Rikkunshito Japanese conventional preparation was superior to domperidone in patients with refractory FD with a Relative Risk (RR) of responding to the symptoms particularly those who had experienced the slow emptying of the gut. Similarly, the anti-inflammatory and antioxidative effect of the bioactive compounds of curcumin was proven in FD and IBS, though there is a problem of standardization. Curcumin bioavailability differs 20 times depending on how it has been prepared and even bioenhancers such as piperine also affect the clinical outcome. The same case on herb-drug interaction: chamomile is administered in such a way that it has a desired effect of producing the dyspeptic effect but in actual effect it may raise the pharmacological effect of anticoagulant which will then escalate to be more bloody. The cultural and dietary conditions also influence the herbal use. The Mediterranean characteristic rich herbs such as oregano, Rosemary and thyme have also been associated with the alleviation of the dyspeptic symptom that is compound both as a dietary and therapeutic benefit (Sperber, et al. 2021).
The comparison tests that have been conducted on the traditional drugs reveal that in most instances the herbs are not inferior to the conventional drugs. To demonstrate the argument, it is determined that the RRs of herbs versus carbapodated drugs in IBS and FD are 1.10 and 1.20, respectively, that is supported by a reduced tolerability and reduced adverse events (Ko, et al. 2021). Mild gastrointestinal upset is the most commonly reported but extreme cases are common (Tan, et al. 2022). The available literature, however, is weak as well. The clinical trials have also been carried out in the Asian population majorly and could not be extrapolated to other ethnicity and dietary conditions. The duration of the trial is also not too long and ranges between 4 to 12 weeks and this may not be able to bring out any long-term effectiveness, compliance trends and safety trends. Besides that, the variability in the herbal preparation, dosage and standardization are also impediments to inter study reproducibility and make it hard to generate evidence based guidelines (Wang, et al. 2021).
The multi-centers, large scale RCTs, standardized herbal preparations and mechanistic biomarkers which are fecal calprotectin in case of inflammation and gut microbiota in case of functional bowel disorders should represent the future perspective of research (Zheng, et al. 2021). The long-term outcomes are also to be examined as well as the probability of the herbs and drugs to interact and the impact of the diet and cultural practices on the accomplishment of the effect. Integration of pharmacodynamics and pharmacokinetic tests will also be descriptive of the dosing, bioavailability and change of responses (Li, et al. 2021). All these could help to enhance the validity and suitability of research on herbal medicine and enable pharmacists and clinicians to generate evidence-based guidance that would be competent enough to be used to optimize the symptoms management, patient safety and the general quality of life of individuals with functional gastrointestinal diseases (Fig. 5) (Zhou, et al. 2021, Salm, et al. 2023).
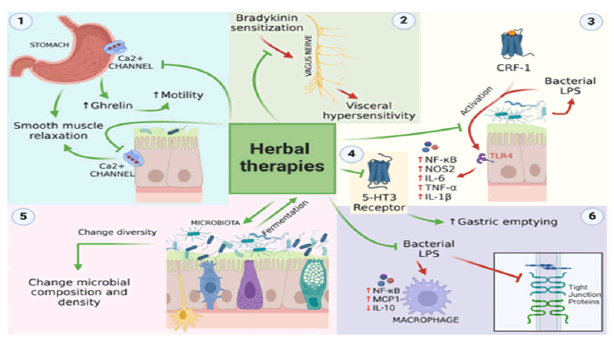
Figure 5. Flowchart of herbal mechanisms in FGIDs.
Conclusion
The mechanisms involved and clinically established efficacy with a number of Functional Gastrointestinal Disorders (FGIDs) attribute the new frontiers in the development of herbal interventions as effective and complementary initiatives in the face of limitations that are related to the standard therapy. One such thing is that peppermint oil has spasmolytic effects in the Irritable Bowel Syndrome (IBS), which relaxes smooth muscle and lowers the visceral hypersensitivity and psyllium fiber corrects bowel regularity in Functional Constipation (FC), which are by bulking and by fermentation-stimulated peristalsis. The polyphenol containing herbs like curcumin have anti-inflammatory and anti-oxidative effects and reduce the symptoms of Functional Dyspepsia (FD) and an overlapping presentation of Functional Gastrointestinal Disease (FGID). In addition to symptomatic, such herbal interventions tend to disrupt more than one pathophysiological pathway, to recompense any dis-connections which might exist between the interventions and single-efficacy pharmaceuticals. The fact that they are integrated in the care of the patients also triggers their cultural practices and eating habits and increases their acceptability and adherence. Nevertheless, to maximize their participation, achieve uniform quality and to create evidence-based clinical guidelines to be implemented globally, rigorous and standardized studies, such as multi-center randomized trials and long-term safety assessment, are necessary.
Recommendations
- Initiate with evidence-based herbs: E.g., 200 mg peppermint oil for IBS pain, consulting for dosing.
- Monitor interactions: Avoid turmeric with blood thinners.
- Educate patients: Use standardized products; report AEs.
- Integrate holistically: Combine with low-FODMAP diet for IBS.
- Fund research: Prioritize long-term RCTs on multi-herb synergies.
References
- Alammar N, Salem O, Ahmad M, Al-Saadi S. (2021). Herbal medicine for irritable bowel syndrome: An overview of systematic reviews.
- Alghamdi MA, Alzahrani FA, Alotaibi AH, Alharbi SS. (2023). Integrated traditional herbal medicine in the treatment of gastrointestinal disorder: Usage, knowledge, and perception in Riyadh, Saudi Arabia.
- Bharucha AE, Pimentel M, Lembo A, Rao SSC. (2025). Clinical efficacy of non-pharmacological treatment of functional constipation: A systematic review and meta-analysis.
- Luo X, Wang L, Fang S, Qing X, Jiang T. (2022). Chinese herbal medicine for functional dyspepsia with psychological disorders: A systematic review and meta-analysis. Front Neurosci. 16:933290.
[Crossref] [Google Scholar] [PubMed]
- Chiarioni G, Popa SL, Ismaiel A, Pop C, Dumitrascu DI. (2023). Herbal remedies for constipation-predominant irritable bowel syndrome: A systematic review of randomized controlled trials. Nutrients. 15:4216.
[Crossref] [Google Scholar] [PubMed]
- Valizadeh R, Mohammad-Alizadeh-Charandabi S, Hajizadeh K, Araj-Khodaei M, Mirghafourvand M. (2025). The effect of combined fig-Walnut syrup on functional constipation in pregnant women: a randomized controlled trial. Nutr Metabol. 22:3.
[Crossref] [Google Scholar] [PubMed
- Rao WW, Yang JJ, Qi H, Sha S, Zheng W. (2021). Efficacy and safety of traditional Chinese herbal medicine for antipsychotic-related constipation: A systematic review and meta-analysis of randomized controlled trials. Front Psych. 12:610171.
[Crossref] [Google Scholar] [PubMed]
- Ho L, Zhong CC, Wong CH, Wu JC, Chan KK, Wu IX. (2022). Herbal medicine for functional dyspepsia: Network meta-analysis of placebo-controlled randomised trials. J Ethnopharmacol. 283:114665.
[Crossref] [Google Scholar] [PubMed]
- Wang L, Ding X, Yao X, Li P, Zhang F. (2024). Efficacy and safety of Xiangsha liujunzi decoction for functional dyspepsia: A systematic review and meta-analysis. Front Pharmacol. 15:1356899.
[Crossref] [Google Scholar] [PubMed]
- Lopresti AL, Drummond PD, Smith S. (2024). A systematic review of the efficacy and safety of turmeric in treating digestive disorders.
- Lyu Z, Fan Y, Bai Y, Liu T, Zhong LL, Liang HF. (2022). Outcome of the efficacy of Chinese herbal medicine for functional constipation: A systematic review and meta-analysis. World J Clin Cases. 10:4856.
[Crossref] [Google Scholar] [PubMed]
- Mickael ME, Rossi F, Conti F (2024). Mitigating digestive disorders: Action mechanisms of Mediterranean herbal remedies.
- Mohammadbeigi R, Azizi M, Esmaeili H. (2024). The efficacy of a traditional herbal medicine compound for functional dyspepsia: A systematic review and meta-analysis.
- Sperber AD, Dumitrascu D, Fukudo S, Gerson C, Ghoshal UC, Mathias R. (2021). Worldwide prevalence of IBS: A rome foundation study. Gastroenterology.
- Ko SJ, Park J, Kim MJ, Kim J, Park JW. (2021). Effects of the herbal medicine Rikkunshito, for functional dyspepsia: A systematic review and metaâanalysis. J Gastroenterol Hepatol. 36:64-74.
[Crossref] [Google Scholar] [PubMed]
- Tan N, Li, H, Wang Y, Chen X. (2022). Systematic review and meta-analysis of Chinese herbal formula Tongxie Yaofang for diarrhea-predominant irritable bowel syndrome.
- Wang L, Zhang Q, Li Y, Zhou H. (2021). Mechanisms of action and clinical effectiveness of herbal treatments for DGBI. Digestive Liver Dis.
[Crossref] [Google Scholar] [PubMed]
- Zheng H, Jin S, Shen YL, Peng WY, Ye K. (2021). Chinese herbal medicine for irritable bowel syndrome: A meta-analysis and trial sequential analysis of randomized controlled trials. Front Pharmacol. 12:694741.
[Crossref] [Google Scholar] [PubMed]
- Li M, Zhao L, Ma L, Zhang W, Huang H. (2021). Efficacy and safety of maxing xianchang su in the treatment of functional constipation: A randomized controlled trial. Evid Complementary Alterna Med. 3685440.
- Zhou Q, Li Y, Xu W (2021). Xiaoyao-san for IBS: Protocol for systematic review and meta-analysis.
- Salm S, Rutz J, van den Akker M, Blaheta RA, Bachmeier BE. (2023). Current state of research on the clinical benefits of herbal medicines for non-life-threatening ailments. Front Pharmacol. 14:1234701.
[Crossref] [Google Scholar] [PubMed]