Review Article - Modern Phytomorphology ( 2025) Volume 19, Issue 6
Comparative meta-analysis of complications in implantable port catheters versus peripherally inserted central catheters in chemotherapy-treated cancer patients
Mohamed S. Imam1*, Jawaher A. Ajeebi2, Manal khaled Saeed Alharthi3, Bayan Sami Altalhi3, Raghad Sultan Alosaimi3, Ghada Attaih Alzahrani3, Layan Wadea Saad Alosaimi3, Hawra Redha Abuayfah3, Faisal Abdulaziz Abdullah Alshareef4, Wajin Rubayyi Q. Alruwely5, Waad Mohammed Abdullah Alamri6, Nasser Mutiq Almuthaybiri7, Khalid Sinhat Alotaibi7, Hussain Ali Abdullah Alhammad8 and Abdulaziz Jameel Saud Alotaibi2College of Pharmacy, Jazan University, Jazan 82912, Saudi Arabia
3College of Pharmacy, Taif University, Taif 21944, Saudi Arabia
4College of Pharmacy, King Khalid University, Abha 62529, Saudi Arabia
5College of Clinical Pharmacy, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
6Al Nahdi Pharmacy, Yanbu, Saudi Arabia
7College of Pharmacy, Shaqra University, Shaqra, Saudi Arabia
8Department of Pharmacy, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia
9Department of Pharmacy, Al-Bejadiyah General Hospital, Ministry of Health, Kingdom of Saudi Arabia
Mohamed S. Imam, Department of Pharmacy, Alnahda College, Riyadh, Kingdom of Saudi Arabia, Email: imammohamed311@gmail.com
Received: 13-May-2025, Manuscript No. mp-25-165485; Accepted: 23-Dec-2025, Pre QC No. mp-25-165485 (PQ); Editor assigned: 15-May-2025, Pre QC No. mp-25-165485 (PQ); Reviewed: 18-Sep-2025, QC No. mp-25-165485; Revised: 24-Nov-2025, Manuscript No. mp-25-165485 (R); Published: 30-Dec-2025, DOI: 10.5281/zenodo.18348387
Abstract
Background and objectives: A meta-analysis compared complications associated with Peripherally Inserted Central Catheters (PICCs) and Implanted Port Catheters (IPCs) in cancer patients undergoing chemotherapy.
Methods: A comprehensive literature search up to December 2024, involving 12,587 participants, was analyzed using pooled Odds Ratios (ORs) and Mean Differences (MDs) with 95% Confidence Intervals (CIs). Dichotomous and continuous outcome measures were evaluated via random-effects or fixed-effects models.
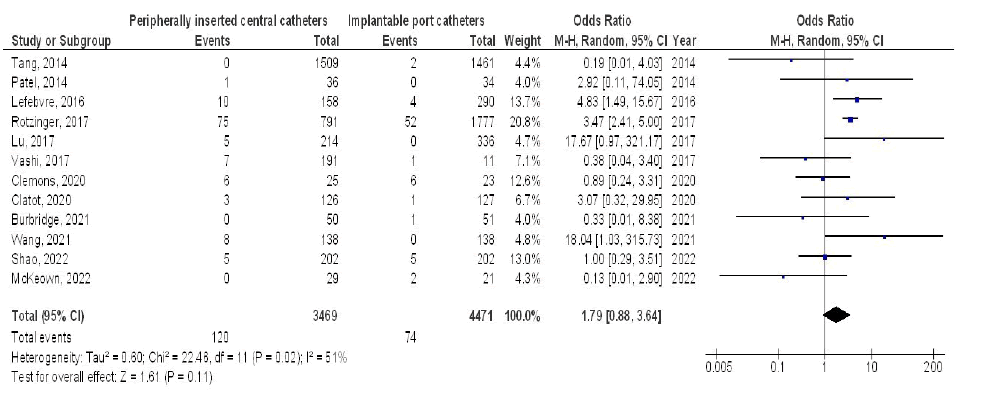
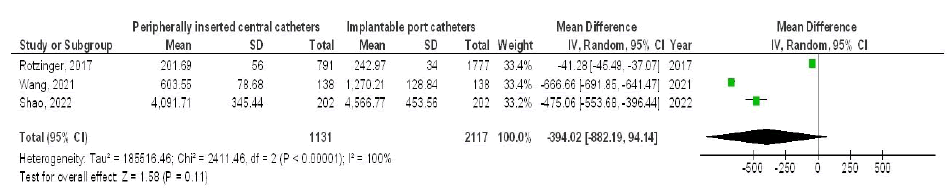
Results: Results revealed that PICC use was linked to significantly elevated risks of occlusion (OR 4.39; 95% CI 2.95-6.52, p<0.001), catheter-related infections (OR 2.42; 95% CI 1.34-4.36, p=0.003), malposition (OR 7.39; 95% CI 3.52-15.50, p<0.001), thrombosis (OR 2.88; 95% CI 2.05-4.05, p<0.001), phlebitis (OR 6.41; 95% CI 2.90-14.14, p<0.001), and accidental removal (OR 3.38; 95% CI 1.97-5.81, p<0.001), alongside a notably shorter indwelling duration (MD -233.16 days; 95% CI -449.52 to -16.80, p=0.03) compared to IPC. However, no significant differences were found in puncture-site local infection rates (OR 1.79; 95% CI 0.88-3.64, p=0.11) or cost (MD -394.02; 95% CI -882.19 to 94.14, p=0.11) between the two devices.
Conclusion: Patients with PICCs experienced significantly more complications than those with IPCs, especially cancer patients undergoing chemotherapy. These complications included occlusions, catheter-related infections, malposition, catheter-related thrombosis, phlebitis, accidental removal, and shorter catheter lifespan. While IPC users experienced fewer of these issues, local insertion site infection duration and costs were comparable between the two groups.
However, the limited sample sizes in seven of the 31 studies included, and the small number of studies contributing to some comparisons, warrants cautious interpretation of these results.
Keywords
Cancer, Chemotherapy, Implanted port catheters, Peripherally inserted central catheters, Catheter-related difficulties, Phytomorphology bioactives, Plant antimicrobials, Medicinal antithrombotics
Introduction
Cancer is currently the second most prevalent cause of death around the world. In China, there are more than 6 million newly diagnosed cancer cases reported each year. Projections indicate that the number of individuals diagnosed with cancer will continue to grow in the future, influenced by shifts in environmental and lifestyle conditions. Chemotherapy remains a standard treatment option for cancer, capable of prolonging the life expectancy of those suffering from metastatic forms of the disease (Ang, et al. 2000). Many chemotherapy regimens are administered through intravenous routes, which may adversely affect peripheral blood vessels. Consequently, central venous access is considered more advantageous than peripheral vascular access, given that frequent venipuncture can result in discomfort for individuals (Silvestri, et al. 2004). Central venous access provides enhanced security and comfort for cancer subjects undergoing chemotherapy. The two common methodologies for administering chemotherapy through this access are Peripherally Inserted Central Catheters (PICC) and Implanted Port Catheters (IPCs) (Johansson, et al. 2013). Peripherally Inserted Central Catheters (PICCs), a type of central venous catheter inserted into arm veins, were first developed in the 1970s. The 1980s saw the creation of Implanted Port Catheters (IPCs), which are placed in the subclavian vein and offer intravenous access without external lines. These advancements in catheter technology have greatly benefited cancer patients, providing a reliable way to receive chemotherapy, long-term infusions, blood tests, and nutritional support. Consequently, nurses often inquire about comparative studies between these two access methodologies (Silvestri, et al. 2004). The issues of patient safety and the growing consciousness regarding costs are critical in the current era. Research is now predominantly aimed at comparing the safety of these two commonly utilized infusion catheters (Rotzinger, et al. 2017). Decision-makers in the medical field are looking forward to obtaining more data to conduct a thorough evaluation of the risks and financial implications of these two surgical procedures. Nevertheless, no substantial or definitive research indicates which central venous catheter is safer. The application of these two catheters varies across different countries, with healthcare professionals more often suggesting the use of peripherally implanted central venous catheters. This trend may be attributed to the belief that peripherally implanted central venous catheters have complication rates that are comparable to those of IPC, along with their lower implantation costs (Tan, et al. 2016). Other studies have specified that the long-term expenses of PICC maintenance may be even higher than those of IPC. Further research has revealed that the long-term costs related to the upkeep of PICCs could be greater than those for IPC. One study showed a higher complication rate for PICCs (32.8%) compared to IPCs. However, another study found similar rates of difficulty during catheterization procedures for both types of catheters (O’Brien, et al. 2013, Walshe, et al. 2002, Worth, et al. 2009). Common complications associated with Peripherally Inserted Central Catheters (PICCs) and implanted port catheters (IPCs) (Chan, et al. 2017).
From an interdisciplinary perspective, phytomorphological research provides insight into how plant structural features underpin the biosynthesis of bioactive compounds with antimicrobial and anti-inflammatory properties, which may conceptually relate to infection and inflammatory complications in clinical settings (Pacyga, et al. 2024).
Description of objectives
Currently, there’s not enough solid evidence to help doctors and patients choose the best catheter. To enhance clinical decision- making, this meta-analysis evaluates the difficulties associated with IPC and PICCs in patients undergoing chemotherapy for cancer. Secondarily, the findings are briefly interpreted within a phytomorphological framework to provide interdisciplinary context.
Methods
Eligibility criteria
The main goal of this investigation was to assess the effects of difficulties associated with IPC and PICC in patients undergoing chemotherapy for cancer. Additionally, a comparative analysis of the two types of catheters was conducted to summarize the findings.
Data sources
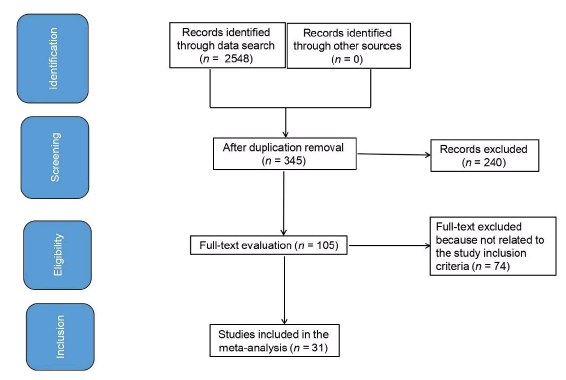
The primary objectives of the present meta-analysis were to assess the difficulties associated with IPC and PICC in patients undergoing chemotherapy for cancer, as well as to investigate the implications of various outcomes. All studies included were conducted on human subjects and were published in any language. The size of the study did not influence its eligibility for inclusion. Review publications, commentaries, and other reports lacking a degree of connotation were omitted from the publication list. Fig.1 illustrates the comprehensive timeline of the study. Publications were included in the meta-analysis when they met the next specifications:
Figure 1: Flowchart of study selection following PRISMA guidelines.
1.The research design was prospective, observational, controlled, or retrospective.
2.Aimed populace comprised chemotherapy-treated cancer subjects.
3. ntervention involved IPC and PICC.
4.The study involved a comparison between IPC and PICCs.
Studies that did not focus on the difficulties arising from PICC and IPC in chemotherapy patients, those involving patients without these catheter types, or studies that did not emphasize the significance of comparative outcomes were omitted from the analysis.
Search strategy
Guided by the PICOS framework, a search strategy protocol was established, structured as follows: P (population): cancer patients undergoing chemotherapy; I (intervention/exposure): PICC and IPC; C (comparison): A comparison of PICC with IPC; O (outcome): difficulties of catheter functionality; S (study design): No restrictions applied (Liberati, et al. 2009). To begin, we performed a detailed search of the Embase, OVID, PubMed, Google Scholar and Cochrane Library databases, with a cutoff date of March 2022. This search incorporated a range of keywords and related terms as presented in Tab.1. To exclude studies that didn’t examine the relationship between PICC and IPC use after cancer chemotherapy.
| Database | Research strategy |
|---|---|
| Pubmed | #1 «cancer using chemotherapy»[MeSH Terms] OR «peripherally inserted central catheters»[All Fields] OR «occlusion difficulties»[All Fields] OR «catheter-related thrombosis «[All Fields] #2 «implanted port catheters»[MeSH Terms] OR «cancer using chemotherapy»[All Fields] OR «catheter-related thrombosis»[All Fields] OR «occlusion difficulties»[All Fields] OR «malposition difficulties»[All Fields] #3 #1 AND #2 |
| Embase | ‘cancer using chemotherapy’/exp OR ‘peripherally inserted central catheters’/exp OR ‘occlusion difficulties’/exp OR ‘catheter-related thrombosis’ #2 ‘implanted port catheters’/exp OR ‘occlusion difficulties’/exp OR ‘malposition difficulties’/exp Or ‘catheter-related thrombosis’ #3 #1 AND #2 |
| Cochrane library |
(cancer using chemotherapy):ti,ab,kw (peripherally inserted central catheters):ti,ab,kw OR (occlusion difficulties) :ti,ab,kw (Word variations have been searched) #2 (catheter-related thrombosis):ti,ab,kw OR (implanted port catheters):ti,ab,kw OR (occlusion difficulties) :ti,ab,kw OR (malposition difficulties) :ti,ab,kw OR (catheter-related thrombosis) :ti,ab,kw (Word variations have been searched) #3 #1 AND #2 |
Table 1. Summary of database search strategies.
Selection process
Following the epidemiological declaration, a methodology was established, which was then systematically organized and evaluated through a meta-analysis.
Data collection process
The data were compiled by established criteria, which included standardized characteristics related to the study and subjects, the last name of the lead author, the study duration, the year of publication, the country and region of the study, the type of population, clinical and treatment characteristics, categorization, methodologies of qualitative and quantitative assessment, sources of information, evaluation of outcomes, and the statistical methodologies used (Page, et al. 2021).
Data items
In cases where a single study produced varying results, we conducted independent data collection focused on evaluating the difficulties related to PICC and IPC in chemotherapy-treated cancer subjects.
Study risk of bias assessment
The two authors independently assessed the methodological quality of the selected research to ascertain the potential for bias within each study. The evaluation of method quality was conducted utilizing the “risk of bias instrument” as outlined in the Cochrane handbook for systematic reviews of interventions version 5.1.0 (Higgins, et al. 2011). The evaluation of each study was conducted by specific criteria, resulting in one of three classifications of bias risk: A low-risk classification was given when all quality criteria were satisfactorily met; an unclear risk classification was assigned when one or more quality criteria were only partially fulfilled or ambiguous; and a high-risk classification was applied when one or more criteria were not satisfied or were absent. The original article was reexamined to rectify any inconsistencies. Botanical sources were not subjected to this risk of bias instrument because they were not included in the statistical meta-analysis but rather served as complementary interpretive material.
Effect measures
Only those studies that described and investigated the effects of PICC on IPC were included in sensitivity analyses. These comparisons were employed for conducting sensitivity and subclass analyses.
Synthesis methodologies, reporting bias assessment, and certainty assessment
We performed a meta-analysis using either a random-effects or a fixed-effects model. Dichotomous and continuous data were analyzed to calculate the Odds Ratio (OR) and Mean Difference (MD), both with 95% Confidence Intervals (CI). The degree of heterogeneity between studies was evaluated using the I² statistic. An I² value of approximately 0% indicated no heterogeneity; 25%, low heterogeneity; 50%, moderate heterogeneity; and 75%, high heterogeneity (Sheikhbahaei, et al. 2016). For this analysis, the statistical model selection was determined by the degree of heterogeneity, as measured by I². If I² was greater than 50%, indicating substantial heterogeneity, a random-effects model was used. Conversely, a fixed-effects model was selected if I² was less than or equal to 50%. A subcategory analysis was conducted by stratifying the data according to pre-established outcome categories. Differences between subcategories were considered statistically significant if the p-value was less than 0.05. Publication bias was investigated using both qualitative methods, examining funnel plots of the log odds ratios, and quantitative methods, employing the Egger regression test. A p-value below 0.05 in the Egger test signified significant publication bias (Higgins, et al. 2003). The calculation of all p-values was performed using two-tailed tests. Reviewer manager version 5.3 was utilized for the statistical analyses and the creation of graphs, as provided by the Nordic Cochrane centre, affiliated with the Cochrane collaboration in Copenhagen, Denmark.
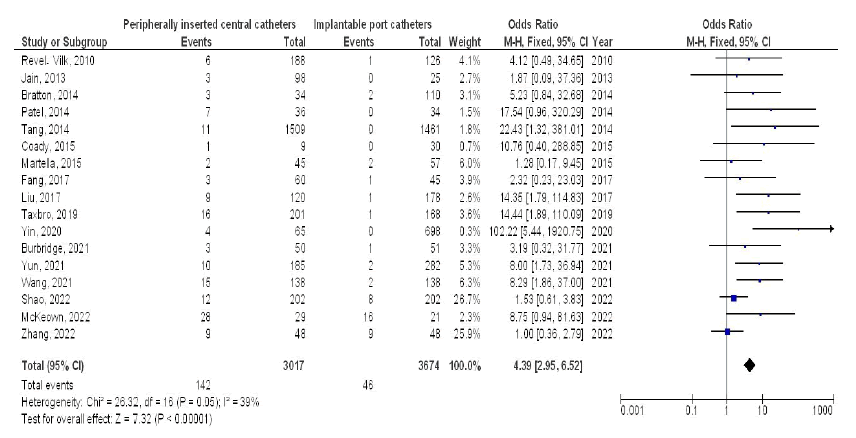
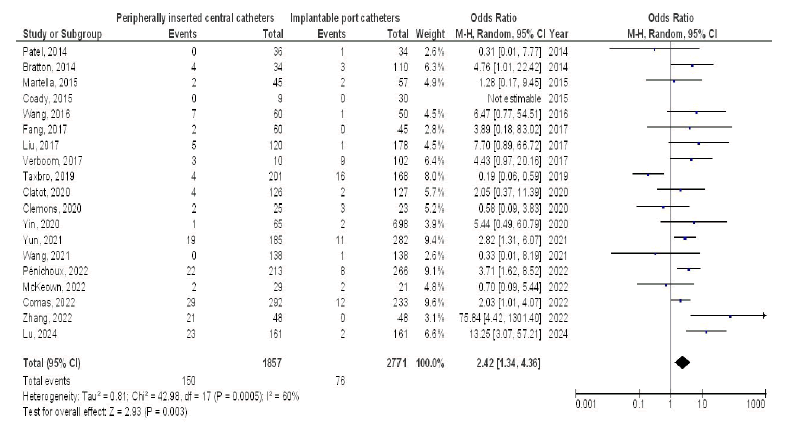
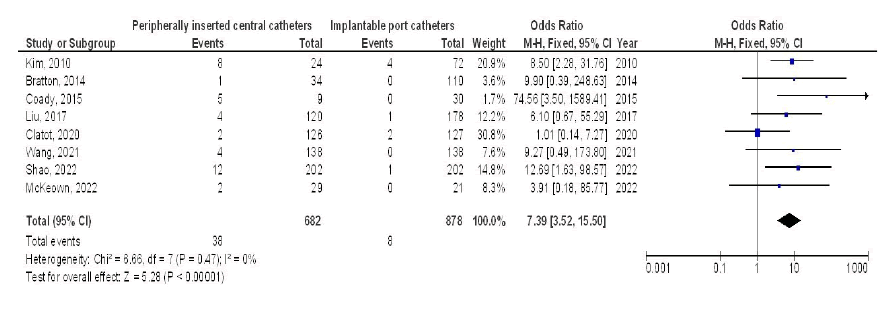
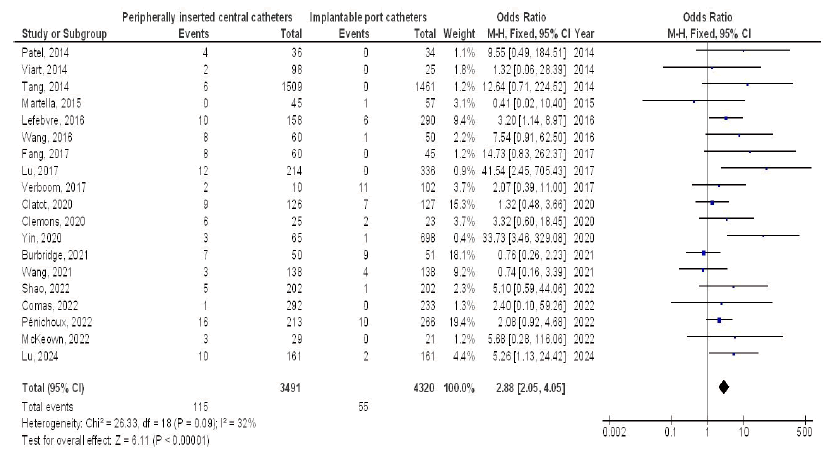
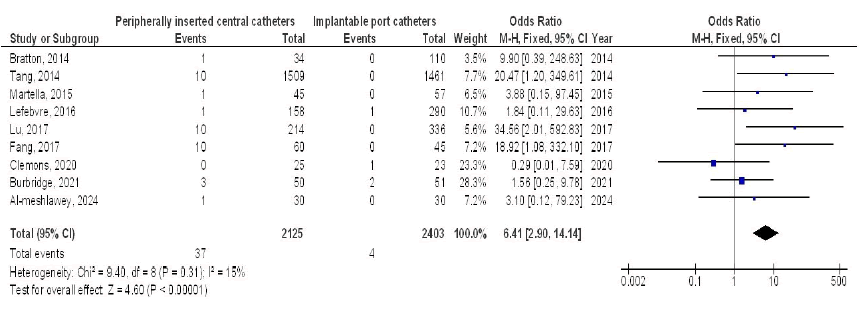
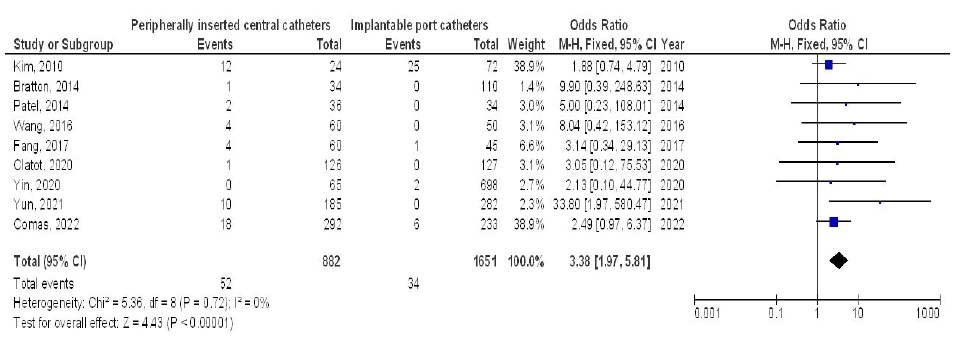
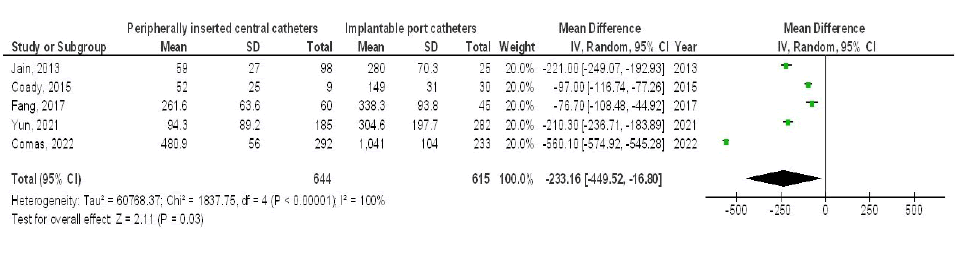
Results
The meta-analysis incorporated 28 articles that satisfied the inclusion criteria, selected from a comprehensive review of 2,548 relevant studies conducted between 2010 and 2024 (Rotzinger, et al. 2017, RevelâVilk, et al. 2010, Kim, et al. 2010, Jain, et al. 2013, Patel, et al. 2014, Viart, et al. 2014, Bratton, et al. 2014, Tang, et al. 2014, Martella, et al. 2015, Coady, et al. 2015, Wang, et al. 2016, Lefebvre, et al. 2016, Verboom, et al. 2017, Fang, et al. 2017, Lu, et al. 2017, Liu, et al. 2017, Vashi, et al. 2017, Taxbro, et al. 2019, Clemons, et al. 2020, Yin and Li, 2020, Clatot, et al. 2020, Wang, et al. 2021, Burbridge, et al. 2021, Yun and Yang, 2021, Comas, et al. 2022, Zhang, et al. 2022, Pénichoux, et al. 2022, McKeown, et al. 2022, Shao, et al. 2022, Lu, et al. 2024, Al-meshlawey, et al. 2024). Tab 2 presents the findings from the aforementioned studies. The selected research involved a total of 11,801 cancer subjects undergoing chemotherapy at the outset; among these, 5,017 utilized PICC, while 7,177 employed IPC. Compared to patients using IPCs, those with PICCs demonstrated a statistically significant increased risk of several complications. These included occlusions (OR 4.39, 95% CI 2.95-6.52, p<0.001, low heterogeneity), catheter-related infections (OR 2.42, 95% CI 1.34-4.36, p=0.003, moderate heterogeneity), malposition difficulties (OR 7.39, 95% CI 3.52-15.50, p<0.001, no heterogeneity), catheter-related thrombosis (OR 2.88, 95% CI 2.05-4.05, p<0.001, moderate heterogeneity), phlebitis (OR 6.41, 95% CI 2.90-14.14, p<0.001, no heterogeneity), and accidental removal (OR 3.38, 95% CI 1.97-5.81, p<0.001, no heterogeneity). Furthermore, PICC lines exhibited a significantly shorter lifespan (MD -233.16, 95% CI -449.52 to -16.80, p=0.03, high heterogeneity). Figs. 2 to 10 provide further details.
| Study | Country | Total | Peripherally inserted central catheters | Implanted port catheters |
|---|---|---|---|---|
| RevelâVilk, 2010 | Israel | 314 | 188 | 126 |
| Kim, 2010 | Korea | 96 | 24 | 72 |
| Jain, 2013 | India | 123 | 98 | 25 |
| Patel, 2014 | Australia | 70 | 36 | 34 |
| Viart, 2014 | France | 123 | 98 | 25 |
| Bratton, 2014 | USA | 144 | 34 | 110 |
| Tang, 2014 | China | 2970 | 1509 | 1461 |
| Martella, 2015 | Italy | 102 | 45 | 57 |
| Coady, 2015 | UK | 39 | 9 | 30 |
| Wang, 2016 | China | 110 | 60 | 50 |
| Lefebvre, 2016 | France | 448 | 158 | 290 |
| Rotzinger, 2017 | Switzerland | 2568 | 791 | 1777 |
| Verboom, 2017 | Netherlands | 112 | 10 | 102 |
| Fang, 2017 | China | 105 | 60 | 45 |
| Lu, 2017 | China | 550 | 214 | 336 |
| Liu, 2017 | China | 298 | 120 | 178 |
| Vashi, 2017 | USA | 202 | 191 | 11 |
| Taxbro, 2019 | Sweden | 369 | 201 | 168 |
| Clemons, 2020 | Canada | 48 | 25 | 23 |
| Yin, 2020 | China | 763 | 65 | 698 |
| Clatot, 2020 | France | 253 | 126 | 127 |
| Wang, 2021 | China | 276 | 138 | 138 |
| Burbridge, 2021 | Canada | 101 | 50 | 51 |
| Yun, 2021 | Korea | 467 | 185 | 282 |
| Comas, 2022 | Spain | 525 | 292 | 233 |
| Zhang, 2022 | China | 96 | 48 | 48 |
| Pénichoux, 2022 | France | 479 | 213 | 266 |
| McKeown, 2022 | USA | 50 | 29 | 21 |
| Shao, 2022 | China | 404 | 202 | 202 |
| Lu, 2024 | China | 322 | 161 | 161 |
| Al-meshlawey, 2024 | Egypt | 60 | 30 | 30 |
| Total | 12587 | 5410 | 7177 |
Table 2. Characteristics of the selected studies for the meta-analysis.
Figure 2: The effect’s forest plot of peripherally inserted central catheters compared with implanted port catheters on occlusion difficulties outcomes in cancer subjects using chemotherapy.
Figure 3: Forest plot comparison of PICCs and IPCs catheter-related infection outcomes in cancer patients receiving chemotherapy.
Figure 4: Forest plot comparing PICC and IPC malposition rates in cancer patients undergoing chemotherapy.
Figure 5: Forest plot comparing PICC and IPC thrombosis rates in cancer patients receiving chemotherapy.
Figure 6: Forest plot of comparing PICC and IPC phlebitis outcomes in cancer patients undergoing chemotherapy.
Figure 7: Forest plot comparing PICC and IPC accidental removal rates in cancer patients receiving chemotherapy
Figure 8: Forest plot comparing PICC and IPC catheter lifespan outcomes in cancer patients undergoing chemotherapy.
Figure 9: Forest plot comparing PICC and IPC local infection duration outcomes in cancer patients undergoing chemotherapy.
Figure 10: Forest plot comparing PICC and IPC treatment costs in chemotherapy.
Discussion
The meta-analysis comprised 11,801 cancer subjects receiving chemotherapy at the start of the studies. Of these patients, 5,017 were using PICC, and 7,177 were utilizing IPC (Rotzinger, et al. 2017, RevelâVilk, et al. 2010, Kim, et al. 2010, Jain, et al. 2013, Patel, et al. 2014, Viart, et al. 2014, Bratton, et al. 2014, Tang, et al. 2014, Martella, et al. 2015, Coady, et al. 2015, Wang, et al. 2016, Lefebvre, et al. 2016, Verboom, et al. 2017, Fang, et al. 2017, Lu, et al. 2017, Liu, et al. 2017, Vashi, et al. 2017, Taxbro, et al. 2019, Clemons, et al. 2020, Yin and Li, 2020, Clatot, et al. 2020, Wang, et al. 2021, Burbridge, et al. 2021, Yun and Yang, 2021, Comas, et al. 2022, Zhang, et al. 2022, Pénichoux, et al. 2022, McKeown, et al. 2022, Shao, et al. 2022, Lu, et al. 2024, Al-meshlawey, et al. 2024). This study found that PICCs, compared to IPCs, led to more complications in cancer patients receiving chemotherapy. Specifically, PICC users experienced higher rates of occlusions, infections, malposition, thrombosis, phlebitis, accidental removals, and shorter catheter lifespans. However, local infection rates at the insertion site and the costs associated with each catheter type were comparable. The limited sample size of 7 out of 31 with fewer than 100 participants and the few studies available for various comparisons necessitate caution in interpreting these findings. This analysis incorporated 28 cohort studies involving over 10,000 cancer subjects receiving chemotherapy, following a comprehensive literature review.
Practitioners need to select the appropriate catheter type based on the patient’s physical condition, expected catheter lifespan, complication rates, and other relevant factors (Kim, et al. 2010). The diminished life expectancy of PICC relative to the IPC could be due to the elevated rates of difficulties connected with the PICC, along with a greater frequency of unintentional removals (Kabsy, et al. 2010). Current infusion therapy standards (2021) state that PICCs are appropriate for use for several months and may remain in place for as long as one year (Gorski, et al. 2021). A variety of studies have confirmed that with diligent maintenance by nurses, an implanted port catheter can be employed for an extended period, often spanning several years (Kock, et al. 1998). In addition, utilizing an implanted port catheter can help reduce the discomfort associated with frequent punctures for patients receiving treatment for more than a year.
The study found that the overall occurrence of all seven difficulties assessed was higher with a peripherally implanted central venous catheter than with an IPC. The presence of cancer, along with chemotherapy treatments delivered through central venous catheters, increases the likelihood of thrombosis and obstruction of vessels or lines (Singh, et al. 2017). The meta-analysis showed that implanted port catheters (IPCs) resulted in less central venous catheter thrombosis and occlusion compared to Peripherally Inserted Central Catheters (PICCs). These results were consistent with those of another systematic review that investigated risk factors for catheter-related thrombosis in cancer patients (Saber, et al. 2011).
The differences in performance between PICCs and IPCs may be attributed to several factors. The longer catheter required for peripheral insertion leads to a more extensive vessel entry, while the IPC’s shorter trajectory results in reduced stimulation of the vessel walls. This mechanical interaction with vascular endothelial cells by an external object may promote the activation of thrombotic factors, which can contribute to vessel blockage. Additionally, the findings of this study revealed that the occurrence of extravasation, malposition, unintentional removal, and phlebitis was significantly lower for IPCs compared to their peripherally inserted counterparts. The anchoring of the IPC base to the chest wall provides a stable access point that is less likely to be affected by upper limb movements. Conversely, the puncture site for a PICC is often located in the arm, increasing the risk of migration during physical exertion or mobility.
The subgroup analysis indicated a higher rate of infection connected with PICCs compared to IPCs. According to Bouza, et al. 2002., PICCs have an external part, they offer a potential entry point for bacteria, increasing the risk of bloodstream or subcutaneous infections. IPCs, being entirely under the skin, eliminate this risk. Additionally, the difficulties arising from PICCs appear to be more significant than those associated with IPC, resulting in increased treatment costs. This context clarifies why IPC generally have lower long-term costs compared to their peripherally inserted counterparts, a finding supported by the cost analysis led by Patel, et al. 2014. His meta-analysis revealed the effects of issues related to peripherally positioned central catheters and IPC on patients with cancer who are receiving chemotherapy.
Further research is necessary to elucidate these possible relationships and to compare the impact of Peripherally Inserted Central Catheters (PICCs) versus Implanted Port Catheters (IPCs) on clinical outcomes. Studies with larger, more standardized cohorts would enhance the validity of findings. This aligns with prior meta-analytic evidence suggesting that PICCs may offer advantages, such as reduced puncture-site infection rates and improved occlusion management (Pu, et al. 2020, Capozzi, et al. 2021, Jiang, et al. 2020, Schears, et al. 2021, Wang, et al. 2022, He, et al. 2021, Balsorano, et al. 2020, Liu, et al. 2021). Our meta-analysis found no connection between age or ethnicity and the outcomes. Further research, particularly well-designed randomized controlled trials, is needed to explore these factors, including interactions between gender, age, ethnicity, and other patient characteristics.
From an interdisciplinary standpoint, phytomorphological research describes how plant structural features underlie the production of antimicrobial, anti-inflammatory, and antithrombotic compounds. While not evaluated in this meta-analysis, such concepts may offer contextual relevance for future supportive strategies addressing catheter-related complications.
Limitations
A significant number of the studies identified in this research were not incorporated into the meta-analysis, which raises concerns regarding potential selection bias. The studies that were excluded did not fulfill the criteria necessary for addition in our study. Six of the 28 studies had sample sizes below 100, which could potentially limit the power of those studies. Furthermore, we were incapable to ascertain the extent to which age and ethnicity may have influenced the outcomes. This study intended to assess the difficulties connected with PICC and IPC in patients undergoing chemotherapy for cancer. Analysis relied on data from prior studies, which might have produce bias owing to the presence of incomplete or inaccurate information. Factors such as the nutritional status of respondents, along with their gender, age, and sex characteristics, could also represent potential sources of bias. Unfortunately, the existence of unpublished articles and missing data may further distort the findings of this research.
Additionally, the phytomorphological perspective was conceptual and not subjected to quantitative analysis.
Conclusion
Patients with PICCs experienced significantly more complications than those with IPCs, especially cancer patients undergoing chemotherapy. These complications included occlusions, catheter-related infections, malposition, catheter-related thrombosis, phlebitis, accidental removal, and shorter catheter lifespan. While IPC users experienced fewer of these issues, local insertion site infection duration and costs were comparable between the two groups. However, the limited sample sizes in seven of the 31 studies included, and the small number of studies contributing to some comparisons, warrants cautious interpretation of these results. Brief consideration of phytomorphological principles provides interdisciplinary context but does not alter the clinical conclusions of this analysis.
Author Contributions
Conceptualization: Mohamed S. Imam; Data curation: All authors; Writing-original draft preparation: All authors; Writing-review and editing: All authors.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Al-meshlawey MA, Abd El-Rahman AE, Hamed MH. (2024). Comparative study between Portacath placement in the central or peripheral veins for chemotherapy. Int J Med Arts. 6:5106-5115.
- Ang P, Chia KH, Teoh MK, Wong KK. (2000). Use of a peripherally implanted subcutaneous permanent central venous access device for chemotherapy–the Singapore general hospital experience. Aust N Z J Med. 30:470-474.
[Crossref] [Google Scholar] [PubMed]
- Balsorano P, Virgili G, Villa G, Pittiruti M, Romagnoli S, De Gaudio AR, Pinelli F. (2020). Peripherally inserted central catheter-related thrombosis rate in modern vascular access era-when insertion technique matters: A systematic review and meta-analysis. J Vasc Access. 21:45-54.
[Crossref] [Google Scholar] [PubMed]
- Bouza E, Burillo A, Munoz P. (2002). Catheter-related infections: Diagnosis and intravascular treatment. Clin Microbiol Infect. 8:265-274.
[Crossref] [Google Scholar] [PubMed]
- Bratton J, Johnstone PA, McMullen KP. (2014). Outpatient management of vascular access devices in children receiving radiotherapy: Complications and morbidity. Pediatr Blood Cancer. 61:499-501.
[Crossref] [Google Scholar] [PubMed]
- Burbridge B, Lim H, Dwernychuk L, Le H, Asif T, Sami A, Ahmed S. (2021). Comparison of the quality of life of patients with breast or colon cancer with an arm vein port (TIVAD) versus a Peripherally Inserted Central Catheter (PICC). Curr Oncol. 28:1495-1506.
[Crossref] [Google Scholar] [PubMed]
- Capozzi VA, Monfardini L, Sozzi G, Armano G, Butera D, Scarpelli E, Barresi G, Benegiamo A, Berretta R. (2021). Peripherally Inserted Central Venous Catheters (PICC) versus totally implantable venous access device (PORT) for chemotherapy administration: A meta-analysis on gynecological cancer patients. Acta Biomed. 92:e2021257.
[Crossref] [Google Scholar] [PubMed]
- Chan RJ, Northfield S, Larsen E, Mihala G, Ullman A, Hancock P, Marsh N, Gavin N, Wyld D, Allworth A, Russell E. (2017). Central venous Access device SeCurement and Dressing Effectiveness for peripherally inserted central catheters in adult acute hospital patients (CASCADE): A pilot randomised controlled trial. Trials. 18:458.
[Crossref] [Google Scholar] [PubMed]
- Clatot F, Fontanilles M, Lefebvre L, Lequesne J, Veyret C, Alexandru C, Leheurteur M, Guillemet C, Gouérant S, Petrau C, Théry JC. (2020). Randomised phase II trial evaluating the safety of peripherally inserted catheters versus implanted port catheters during adjuvant chemotherapy in patients with early breast cancer. Eur J Cancer. 126:116-124.
[Crossref] [Google Scholar] [PubMed]
- Clemons M, Stober C, Kehoe A, Bedard D, MacDonald F, Brunet MC, Saunders D, Vandermeer L, Mazzarello S, Awan A, Basulaiman B. (2020). A randomized trial comparing vascular access strategies for patients receiving chemotherapy with trastuzumab for early-stage breast cancer. Support Care Cancer. 28:4891-4899.
[Crossref] [Google Scholar] [PubMed]
- Coady K, Ali M, Sidloff D, Kenningham RR, Ahmed S. (2015). A comparison of infections and complications in central venous catheters in adults with solid tumours. J Vasc Access. 16:38-41.
[Crossref] [Google Scholar] [PubMed]
- Comas M, Domingo L, Jansana A, Lafuente E, Civit A, García-Pérez L, de la Vega CL, Cots F, Sala M, Castells X. (2022). Cost-effectiveness analysis of peripherally inserted central catheters versus central venous catheters for in-hospital parenteral nutrition. J Patient Saf. 18:e1109-e1115.
[Crossref] [Google Scholar] [PubMed]
- Fang S, Yang J, Song L, Jiang Y, Liu Y. (2017). Comparison of three types of central venous catheters in patients with malignant tumor receiving chemotherapy. Patient Prefer Adherence. 11:1197.
[Crossref] [Google Scholar] [PubMed]
- Gorski LA, Hadaway L, Hagle ME, Broadhurst D, Clare S, Kleidon T, Meyer BM, Nickel B, Rowley S, Sharpe E. (2021). Infusion therapy standards of practice. J Infus Nurs. 44:S1-S224.
[Crossref] [Google Scholar] [PubMed]
- He E, Ye K, Zheng H. (2021). Clinical effect and safety of venous access ports and peripherally inserted central catheters in patients receiving tumor chemotherapy: A systematic review and meta-analysis. Ann Palliat Med. 10:9105-9113.
[Crossref] [Google Scholar] [PubMed]
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, SavoviÄ J, Schulz KF, Weeks L, Sterne JA. (2011). The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 343:d5928.
[Crossref] [Google Scholar] [PubMed]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. (2003). Measuring inconsistency in meta-analyses. BMJ. 327:557-560.
[Crossref] [Google Scholar] [PubMed]
- Jain SA, Shukla SN, Talati SS, Parikh SK, Bhatt SJ, Maka V. (2013). A retrospective study of central venous catheters GCRI experience. Indian J Med Paediatr Oncol. 34:238-241.
[Crossref] [Google Scholar] [PubMed]
- Jiang M, Li CL, Pan CQ, Yu L. (2020). The risk of bloodstream infection associated with totally implantable venous access ports in cancer patient: A systematic review and meta-analysis. Support Care Cancer. 28:361-372.
[Crossref] [Google Scholar] [PubMed]
- Johansson E, Hammarskjöld F, Lundberg D, Arnlind MH. (2013). Advantages and disadvantages of Peripherally Inserted Central Venous Catheters (PICC) compared to other central venous lines: A systematic review of the literature. Acta Oncol. 52:886-892.
[Crossref] [Google Scholar] [PubMed]
- Kabsy Y, Baudin G, Vinti H, Novellas S, Mannone L, Chevallier P, Mounier N. (2010). Peripherally Inserted Central Catheters (PICC) in onco-hematology. PICC line in onco-hematology. Bull Cancer. 97:1067-1071.
[Crossref] [Google Scholar] [PubMed]
- Kim HJ, Yun J, Kim HJ, Kim KH, Kim SH, Lee SC, Bae SB, Kim CK, Lee NS, Lee KT, Park SK. (2010). Safety and effectiveness of central venous catheterization in patients with cancer: Prospective observational study. J Korean Med Sci. 25:1748-1753.
[Crossref] [Google Scholar] [PubMed]
- Kock HJ, Pietsch M, Krause U, Wilke H, Eigler FW. (1998). Implantable vascular access systems: Experience in 1500 patients with totally implanted central venous port systems. World J Surg. 22:12-16.
[Crossref] [Google Scholar] [PubMed]
- Lefebvre L, Noyon E, Georgescu D, Proust V, Alexandru C, Leheurteur M, Thery JC, Savary L, Rigal O, Di Fiore F, Veyret C. (2016). Port catheter versus peripherally inserted central catheter for postoperative chemotherapy in early breast cancer: A retrospective analysis of 448 patients. Support Care Cancer. 24:1397-1403.
[Crossref] [Google Scholar] [PubMed]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol. 62:e1-e34.
[Crossref] [Google Scholar] [PubMed]
- Liu B, Wu Z, Lin C, Li L, Kuang X. (2021). Applicability of TIVAP versus PICC in non-hematological malignancies patients: A meta-analysis and systematic review. PloS One. 16:e0255473.
[Crossref] [Google Scholar] [PubMed]
- Liu Y. (2017). Comparison of implanted vascular access ports and PICC in breast cancer patients. Chin J Prac Nurs. 10:1413-1416.
- Lu A, Hu M, Qi X, Zhao Y, Huang Y. (2024). A retrospective cohort study of implantable venous access port-related and peripherally inserted central catheter-related complications in patients with hematological malignancies in China. SAGE Open Med. 12:20503121241257190.
[Crossref] [Google Scholar] [PubMed]
- Lu XT, Gao RF, Zhang YF. (2017). Clinical use of ultrasound-guided implantable venous access port versus PICC in chemotherapy of breast cancer. Chin Remedies Clin. 17:13-16.
- Martella F, Salutari V, Marchetti C, Pisano C, Di Napoli M, Pietta F, Centineo D, Caringella AM, Musella A, Fioretto L. (2015). A retrospective analysis of trabectedin infusion by peripherally inserted central venous catheters: A multicentric Italian experience. Anti-Cancer Drugs. 26:990-994.
[Crossref] [Google Scholar] [PubMed]
- McKeown C, Ricciuti A, Agha M, Raptis A, Hou JZ, Farah R, Redner RL, Im A, Dorritie KA, Sehgal A, Rossetti J. (2022). A prospective study of the use of central venous catheters in patients newly diagnosed with acute myeloid leukemia treated with induction chemotherapy. Support Care Cancer. 30:1673-1679.
[Crossref] [Google Scholar] [PubMed]
- O'Brien J, Paquet F, Lindsay R, Valenti D. (2013). Insertion of PICCs with minimum number of lumens reduces complications and costs. J Am Coll Radiol. 10:864-868.
[Crossref] [Google Scholar] [PubMed]
- Pacyga K, Pacyga P, Topola E, Viscardi S, Duda-Madej A. (2024). Bioactive compounds from plant origin as natural antimicrobial agents for the treatment of wound infections. Int J Mol Sci. 25:2100.
[Crossref] [Google Scholar] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst Rev. 10:89.
- Patel GS, Jain K, Kumar R, Strickland AH, Pellegrini L, Slavotinek J, Eaton M, McLeay W, Price T, Ly M, Ullah S. (2014). Comparison of Peripherally Inserted Central Venous Catheters (PICC) versus subcutaneously implanted port-chamber catheters by complication and cost for patients receiving chemotherapy for non-haematological malignancies. Support Care Cancer. 22:121-128.
[Crossref] [Google Scholar] [PubMed]
- Pénichoux J, Rio J, Kammoun L, Vermeulin T, Pepin LF, Camus V, Dubois S, Bouclet F, Alani M, Contentin N, Leprêtre S. (2022). Retrospective analysis of the safety of peripherally inserted catheters versus implanted port catheters during firstâline treatment for patients with diffuse large Bâcell lymphoma. Eur J Haematol. 109:41-49.
[Crossref] [Google Scholar] [PubMed]
- Pu YL, Li ZS, Zhi XX, Shi YA, Meng AF, Cheng F, Ali A, Li C, Fang H, Wang C. (2014). The maintenance comparison of applying PICC and VPA among cancer patients undergoing chemotherapy. Chin Nurs Manage. 14:420-422.
- Pu YL, Li ZS, Zhi XX, Shi YA, Meng AF, Cheng F, Ali A, Li C, Fang H, Wang C. (2020). Complications and costs of peripherally inserted central venous catheters compared with implantable port catheters for cancer patients: A meta-analysis. Cancer Nurs. 43:455-467.
[Crossref] [Google Scholar] [PubMed]
- RevelâVilk S, Yacobovich J, Tamary H, Goldstein G, Nemet S, Weintraub M, Paltiel O, Kenet G. (2010). Risk factors for central venous catheter thrombotic complications in children and adolescents with cancer. Cancer. 116:4197-4205.
[Crossref] [Google Scholar] [PubMed]
- Rotzinger R, Gebauer B, Schnapauff D, Streitparth F, Wieners G, Grieser C, Freyhardt P, Hamm B, Maurer MH. (2017). Placement of central venous port catheters and peripherally inserted central catheters in the routine clinical setting of a radiology department: analysis of costs and intervention duration learning curve. Acta Radiol. 58:1468-1475.
[Crossref] [Google Scholar] [PubMed]
- Saber W, Moua T, Williams EC, Verso M, Agnelli G, Couban S, Young A, De Cicco M, Biffi R, Van Rooden CJ, Huisman MV. (2011). Risk factors for CatheterâRelated Thrombosis (CRT) in cancer patients: A PatientâLevel Data (IPD) metaâanalysis of clinical trials and prospective studies. J Thromb Haemost. 9:312-319.
[Crossref] [Google Scholar] [PubMed]
- Schears GJ, Ferko N, Syed I, Arpino JM, Alsbrooks K. (2021). Peripherally inserted central catheters inserted with current best practices have low deep vein thrombosis and central line-associated bloodstream infection risk compared with centrally inserted central catheters: A contemporary meta-analysis. J Vasc Access. 22:9-25.
[Crossref] [Google Scholar] [PubMed]
- Shao G, Zhou X, Zhang S, Wu S, Dong Y, Dong Z. (2022). Cost-utility analysis of centrally inserted totally implanted access port (PORT) versus Peripherally Inserted Central Catheter (PICC) in the oncology chemotherapy. Front Public Health. 10:942175.
[Crossref] [Google Scholar] [PubMed]
- Sheikhbahaei S, Trahan TJ, Xiao J, Taghipour M, Mena E, Connolly RM, Subramaniam RM. (2016). FDG-PET/CT and MRI for evaluation of pathologic response to neoadjuvant chemotherapy in patients with breast cancer: a meta-analysis of diagnostic accuracy studies. Oncologist. 21:931-939.
[Crossref] [Google Scholar] [PubMed]
- Silvestri V, Nerini L, Missio G, Masini M, Faggi S, Gori A, Panella M. (2004). Levels of anxiety and pain during chemotherapy with peripheral versus central vascular access: An experimental evaluation. J Vasc Access. 5:147-53.
[Crossref] [Google Scholar] [PubMed]
- Singh G, Rathi AK, Singh K, Sharma D. (2017). Venous thromboembolism in cancer patients–magnitude of problem, approach, and management. Indian J Cancer. 54:308.
[Crossref] [Google Scholar] [PubMed]
- Tan J, Liu L, Xie J, Hu L, Yang Q, Wang H. (2016). Cost-effectiveness analysis of ultrasound-guided Seldinger Peripherally Inserted Central Catheters (PICC). Springerplus. 5:2051.
[Crossref] [Google Scholar] [PubMed]
- Tang P. (2014). The maintenance comparison of applying PICC and VPA among cancer patients undergoing chemotherapy. Chin Nurs Manage. 14:420-422.
- Taxbro K, Hammarskjöld F, Thelin B, Lewin F, Hagman H, Hanberger H, Berg S. (2019). Clinical impact of peripherally inserted central catheters versus implanted port catheters in patients with cancer: an open-label, randomised, two-centre trial. Br J Anaesth. 122:734-741.
[Crossref] [Google Scholar] [PubMed]
- Vashi PG, Virginkar N, Popiel B, Edwin P, Gupta D. (2017). Incidence of and factors associated with catheter-related bloodstream infection in patients with advanced solid tumors on home parenteral nutrition managed using a standardized catheter care protocol. BMC Infect Dis. 17:1-9.
[Crossref] [Google Scholar] [PubMed]
- Verboom MC, Ouwerkerk J, Steeghs N, Lutjeboer J, Martijn Kerst J, van der Graaf WT, Reyners AK, Sleijfer S, Gelderblom H. (2017). Central venous access related adverse events after trabectedin infusions in soft tissue sarcoma patients; experience and management in a nationwide multi-center study. Clin Sarcoma Res. 7:1-6.
[Crossref] [Google Scholar] [PubMed]
- Viart H, Combe C, Martinelli T, Thomas J, Hida H. (2014). Comparison between implantation costs of peripherally inserted central catheter and implanted subcutaneous ports. Ann Pharm Fr. 73:239-244.
[Crossref] [Google Scholar] [PubMed]
- Wang K, Zhou Y, Huang N, Lu Z, Zhang X. (2021). Peripherally inserted central catheter versus totally implanted venous port for delivering medium-to long-term chemotherapy: A cost-effectiveness analysis based on propensity score matching. J Vasc Access. 23:365-374.
[Crossref] [Google Scholar] [PubMed]
- Wang N, Dong Y, Zhang B, Gao YJ, Fu H. (2016). Comparison of the application of IVPA and PICC in breast cancer patients. Med Philos B. 37:36-38.
- Wang P, Soh KL, Ying Y, Liu Y, Huang X, Huang J. (2022). Risk of VTE associated with PORTs and PICCs in cancer patients: A systematic review and meta-analysis. Thromb Res. 213:34-42.
[Crossref] [Google Scholar] [PubMed]
- Walshe LJ. (2002). Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol. 20:3276-3281.
- Worth LJ, Seymour JF, Slavin MA. (2009). Infective and thrombotic complications of central venous catheters in patients with hematological malignancy: prospective evaluation of nontunneled devices. Support Care Cancer. 17:811-818.
[Crossref] [Google Scholar] [PubMed]
- Yin L, Li J. (2020). Central venous catheter insertion in colorectal cancer patients, PICC or PC? Cancer Manag Res. 12:5813.
[Crossref] [Google Scholar] [PubMed]
- Yun WS, Yang SS. (2021). Comparison of peripherally inserted central catheters and totally implanted venous access devices as chemotherapy delivery routes in oncology patients: A retrospective cohort study. Sci Prog. 104:368504211011871.
[Crossref] [Google Scholar] [PubMed]
- Zhang H, Li Y, Zhu N, Li Y, Fu J, Liu J. (2022). Comparison of Peripherally Inserted Central Catheters (PICCs) versus totally implantable venous-access ports in pediatric oncology patients, a single center study. Sci Rep. 12:1-7.